SGOT (serum glutamic-oxaloacetic transaminase), also called aspartate aminotransferase (AST), and SGPT (serum glutamic-pyruvic transaminase), also known as alanine aminotransferase (ALT), are essential liver enzymes routinely assessed in liver function tests. These enzymes are released into the bloodstream when liver cells are damaged, making them crucial biomarkers for detecting liver injury, inflammation, or systemic metabolic stress.
AST and ALT levels help clinicians evaluate liver health and diagnose conditions such as viral hepatitis (Hepatitis B and C), alcohol-related liver disease, and non-alcoholic fatty liver disease (NAFLD), including its more severe form, non-alcoholic steatohepatitis (NASH). Elevated transaminase levels can also indicate medication-induced hepatotoxicity, especially from statins or other hepatically metabolized drugs.
In the UAE, SGOT and SGPT testing is widely used across DHA-accredited laboratories in Dubai and SEHA-governed hospitals in Abu Dhabi. These tests are often included in mandatory health screenings for visa issuance, routine wellness packages, and occupational health protocols such as OSHAD-SF. Healthcare networks like Aster, LLH, Zia, and Burjeel incorporate liver enzyme panels as part of their preventive and diagnostic workflows.
A typical liver panel includes not just AST and ALT, but also other markers like alkaline phosphatase (ALP), gamma-glutamyl transferase (GGT), and bilirubin. However, the AST/ALT ratio—also known as the De Ritis ratio—remains a widely used clinical indicator for differentiating types of liver disease and gauging severity.
Access to liver enzyme testing in the UAE is influenced by insurance plans such as Daman, Thiqa, and Sukoon. Some offer full reimbursement for outpatient diagnostics and chronic disease monitoring, while others limit coverage to basic evaluations. Patients with abnormal enzyme levels may require follow-up tests such as abdominal ultrasound, FibroScan (transient elastography), or non-invasive fibrosis scoring systems like FIB-4 and the NAFLD Fibrosis Score.
SGOT and SGPT testing plays a vital role in early disease detection, risk stratification, and treatment planning. It enables both general practitioners and specialists to make informed clinical decisions—while aligning with regulatory standards set by DOH, DHA, and MOHAP in the UAE healthcare system.
SGOT and SGPT Test Price in UAE (2025)
The average price of an SGOT and SGPT test in the UAE ranges from AED 89 to AED 220, depending on the diagnostic center and whether it’s included in a full liver function test (LFT) panel.
- Redcliffe Labs offers SGOT/SGPT tests starting at AED 89 via home sample collection.
- Aster, LLH, and Burjeel Hospitals offer the test between AED 120 to AED 220, often as part of visa medicals or wellness screenings.
- Government facilities like SEHA and DHA centers may provide the test free of cost under insurance plans such as Thiqa or Daman.
| Lab / Hospital | Location | Test Name | Price (AED) | Booking Info |
|---|---|---|---|---|
| Redcliffe Labs | Online / UAE-wide | SGOT/SGPT (Home Visit) | AED 89–149 | Book via Redcliffe Labs |
| Aster Clinics | Dubai, Sharjah | LFT Panel | AED 120–180 | Book via Aster app or website |
| LLH / Burjeel | Abu Dhabi, Al Ain | LFT (Includes SGPT/SGOT) | AED 180–240 | SEHA-approved; includes report |
| Medeor / Zulekha | Dubai & Northern Emirates | ALT/AST Panel | AED 150–220 | May include consultation |
| SEHA Govt Facilities | Abu Dhabi | ALT/AST (insured) | Free with Thiqa/Daman | For eligible Emiratis / residents |
Always confirm whether fasting is required and if insurance coverage applies before booking your test. Prices may vary slightly between emirates or if bundled with other diagnostics.
What Are SGOT and SGPT Tests?
SGOT and SGPT are liver enzyme tests that assess the presence and severity of hepatocellular injury. These enzymes are released into the bloodstream when liver cells are inflamed or damaged, making them essential biomarkers for diagnosing and monitoring liver health.
SGOT stands for Serum Glutamic Oxaloacetic Transaminase, also referred to in clinical practice as Aspartate Aminotransferase (AST). SGPT stands for Serum Glutamic Pyruvic Transaminase, also known as Alanine Aminotransferase (ALT). Both belong to the aminotransferase group of enzymes and are primarily involved in amino acid metabolism within liver cells.
When liver tissue is injured—due to infections, toxins, medications, or metabolic conditions—these enzymes leak from hepatocytes into the bloodstream. Elevated levels of SGOT and SGPT in a blood test serve as red flags for potential liver dysfunction.
The SGOT and SGPT tests are conducted via venous blood samples and reported in units per liter (U/L). Higher-than-normal values indicate the presence of active liver inflammation, but the pattern of elevation—such as isolated ALT rise or a higher AST/ALT ratio—can provide additional diagnostic insights.
Clinicians routinely use SGOT and SGPT levels to assess liver integrity, guide treatment decisions, and monitor the progression or resolution of hepatic conditions. These tests form a core part of comprehensive liver function panels and are also included in routine health screenings, visa medicals, and occupational health protocols across the UAE healthcare system.
Why Are SGOT and SGPT Tests Ordered?

SGOT and SGPT tests are routinely ordered to evaluate liver health, detect hepatocellular injury, and monitor ongoing liver conditions. Physicians rely on these enzyme markers for both diagnostic and preventive purposes in a wide range of clinical scenarios.
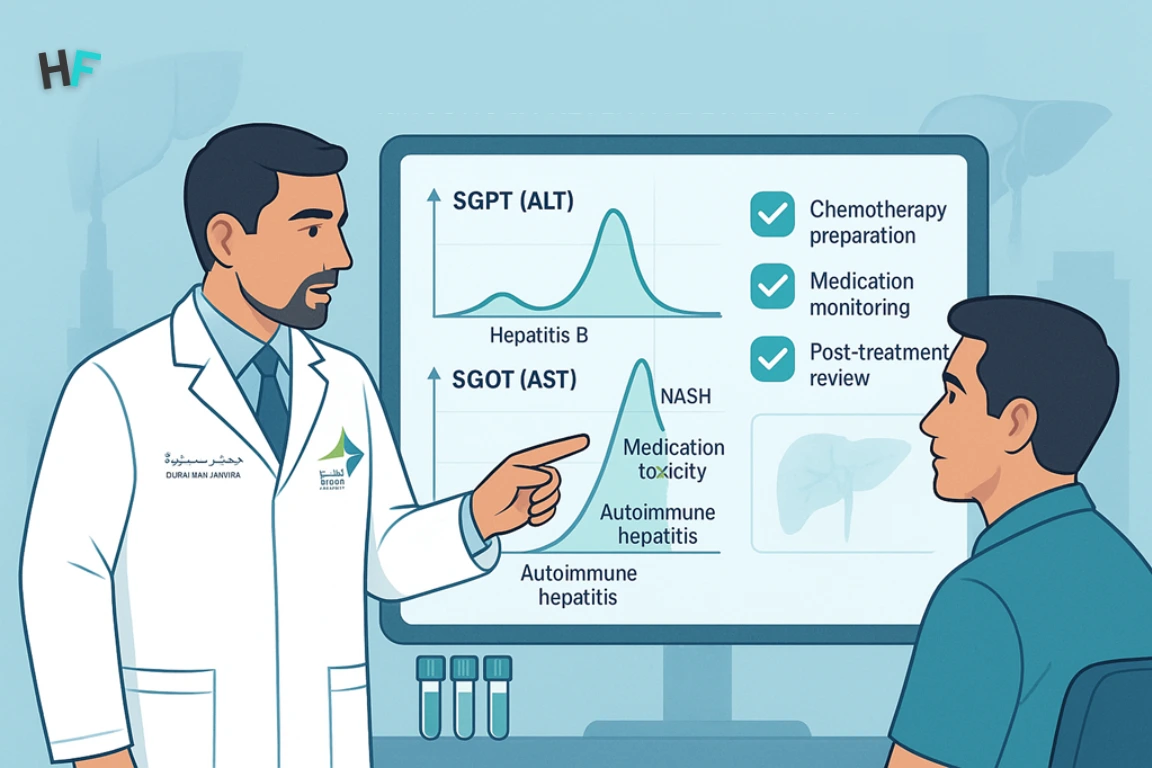
One of the most common reasons for ordering SGOT and SGPT tests is the diagnosis of viral hepatitis, particularly Hepatitis B and Hepatitis C. Elevated transaminase levels often serve as the first biochemical indication of active hepatic inflammation caused by viral replication and immune-mediated hepatocyte destruction.
These tests are also used to monitor the progression of liver damage in chronic conditions such as non-alcoholic steatohepatitis (NASH), alcoholic liver disease, autoimmune hepatitis, and drug-induced liver injury. Regular monitoring helps determine the stage of liver disease and informs decisions about escalation or modification of therapy.
SGOT and SGPT levels are routinely assessed prior to initiating chemotherapy, major surgeries, or long-term medication regimens—especially those involving hepatotoxic agents like statins, antitubercular drugs, or antiepileptics. Baseline values are essential for evaluating liver tolerance and minimizing the risk of adverse reactions.
Additionally, clinicians use these enzyme tests to assess response to treatment in patients already diagnosed with liver disease. A decline in enzyme levels often suggests therapeutic efficacy, while persistently elevated or rising levels may indicate disease progression, inadequate response, or the emergence of complications such as fibrosis or cirrhosis.
Across the UAE healthcare system, SGOT and SGPT assessments are integrated into evidence-based liver disease management protocols, forming a cornerstone of both inpatient and outpatient hepatology workflows.
What Is the Normal Range of SGOT and SGPT Levels?
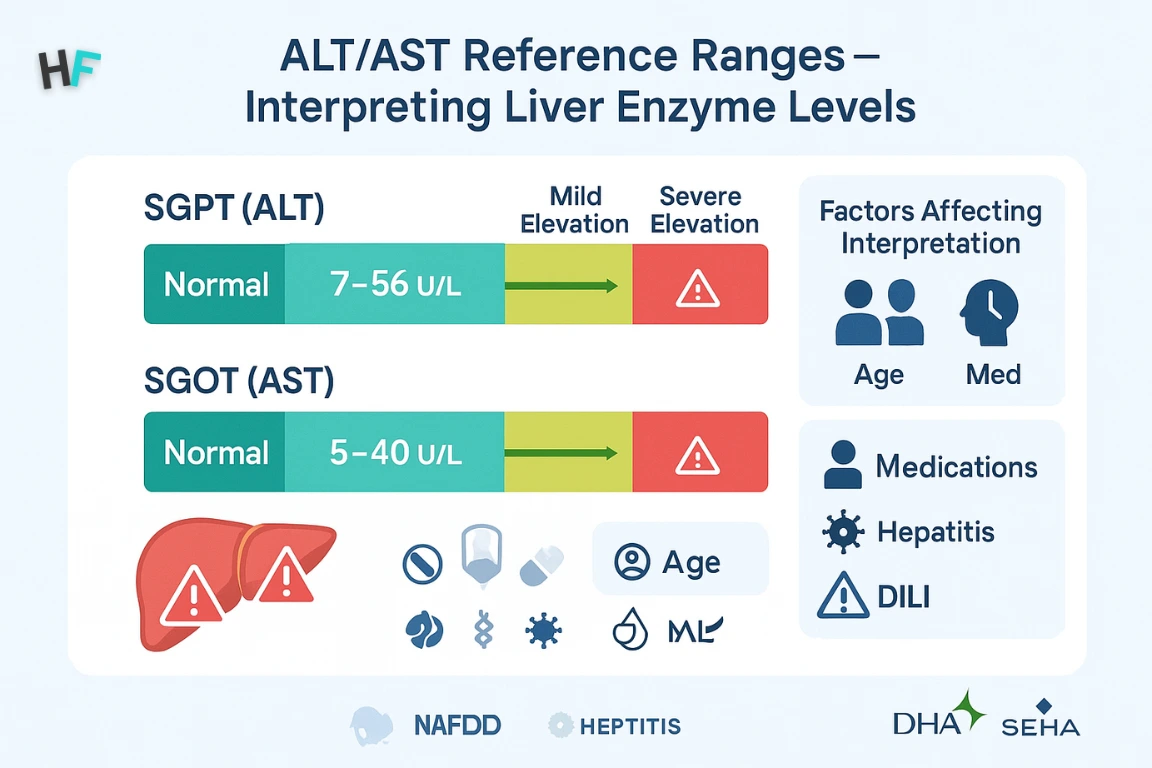
The normal reference range for SGOT (AST) and SGPT (ALT) enzymes provides a baseline for evaluating liver health. These values are used by clinicians to detect abnormalities and interpret liver function status in the context of each patient’s clinical profile.
The typical range for SGOT (AST) is 5 to 40 units per liter (U/L), while the normal range for SGPT (ALT) falls between 7 to 56 U/L. These values reflect enzyme activity in peripheral blood and are measured through standard biochemical assays.
It’s important to note that reference ranges can vary slightly depending on laboratory standards, testing methodologies, age, and gender. For example, males may have slightly higher baseline ALT levels than females, and older adults might show different patterns of transaminase elevation due to age-related hepatic changes.
Elevated SGOT or SGPT levels may suggest underlying liver inflammation or hepatocellular injury. Mild increases can occur with fatty liver, alcohol consumption, or medication use, while significantly elevated values may indicate acute hepatitis, toxic liver injury, or advanced fibrosis.
Laboratory interpretation always requires correlation with other clinical parameters, including bilirubin, alkaline phosphatase, GGT, imaging results, and patient history. Persistent elevations should prompt further investigation to identify the underlying etiology and determine the need for specialist referral.
High SGOT and SGPT – What Do They Indicate?
Elevated levels of SGOT and SGPT in the blood are key indicators of hepatocellular stress or injury. These elevations reflect enzyme leakage from damaged liver cells and serve as biochemical red flags for both acute and chronic liver pathologies.
An elevated SGPT (ALT) level is more specific to hepatocellular injury, as ALT is predominantly localized within liver tissue. Increased ALT is commonly associated with conditions such as viral hepatitis, non-alcoholic steatohepatitis (NASH), and drug-induced liver injury.
In contrast, high SGOT (AST) levels are less liver-specific because AST is also found in cardiac muscle, skeletal muscle, kidneys, and the brain. Elevated AST may therefore be observed not only in liver disease but also in myocardial infarction, muscle trauma, or rhabdomyolysis. As a result, isolated AST elevation warrants broader diagnostic consideration.
The SGOT:SGPT ratio—also known as the De Ritis ratio—is frequently used to differentiate between alcoholic and non-alcoholic liver disease. A ratio greater than 2 is suggestive of alcoholic hepatitis, while a ratio below 1 is more typical in viral hepatitis and metabolic liver disorders.
Extremely high transaminase levels, often above 1000 U/L, are commonly seen in acute viral hepatitis, hepatic ischemia (shock liver), and toxin-induced liver injury. These cases typically require immediate evaluation, imaging studies, and specialist consultation due to the risk of liver failure or systemic complications.
Ultimately, the clinical interpretation of SGOT and SGPT levels depends on the magnitude of elevation, the ratio between them, and the patient’s overall clinical context, including symptoms, comorbidities, and medication use.
Best Medicines for High SGPT and SGOT – Evidence-Based Interventions
Elevated liver enzymes such as SGPT (ALT) and SGOT (AST) are managed based on the underlying etiology, not just the enzyme elevation itself. Below is a structured therapeutic matrix outlining evidence-based pharmacologic options aligned with UAE 2025 protocols and international hepatology guidelines:
| Liver Condition | Recommended Medication(s) | Mechanism of Action | Target Population | Clinical Guideline Source |
|---|---|---|---|---|
| NAFLD / NASH | Pioglitazone, GLP-1 RAs (e.g., Semaglutide), Vitamin E | Insulin sensitization, hepatic fat reduction | T2DM, obesity, metabolic syndrome | EASL, AASLD, MOHAP |
| Viral Hepatitis B / C | Tenofovir, Entecavir, Sofosbuvir-Velpatasvir | Antiviral suppression or viral clearance | HBV or HCV-positive individuals | UAE National Viral Hepatitis Program |
| Drug-Induced Liver Injury | N-acetylcysteine (NAC), Withdrawal of hepatotoxic drugs | Glutathione replenishment, toxin elimination | Paracetamol overdose, polypharmacy patients | WHO, DHA pharmacovigilance guidelines |
| Autoimmune Hepatitis | Prednisolone ± Azathioprine | Immune modulation and inflammation control | ANA/ASMA-positive, idiopathic liver enzyme rise | SEHA, EASL autoimmune liver protocols |
| Alcoholic Liver Disease | Corticosteroids (select cases), micronutrient support | Anti-inflammatory (in severe cases), nutritional rehab | Chronic alcohol users with high Maddrey scores | AASLD, SEHA, DHA clinical care algorithms |
How to Reduce SGOT and SGPT Levels (2025 UAE Protocols)
High SGPT and SGOT levels can often be improved through simple, evidence-based steps. The table below lists common causes of elevation and what you can do—medically and at home—to help bring your liver enzymes back to normal.
| Cause of High Enzymes | What You Should Do | Why It Helps |
|---|---|---|
| No Clear Cause | Repeat test in 2–4 weeks, get an ultrasound or FibroScan | Helps check if the elevation is serious or just temporary |
| Fatty Liver (NAFLD/NASH) | Lose 5–10% of body weight. Add leafy greens, oats, olive oil. Reduce sugar and fried food | Lowers liver fat, improves insulin resistance and inflammation |
| Unhealthy Diet / Obesity | Replace red meat with fish or lean chicken. Cut sugary drinks. Use whole grains | Improves liver metabolism and reduces fat buildup |
| Lack of Exercise | Walk briskly 30–45 minutes a day, 5 times/week or join a fitness class | Physical activity helps burn liver fat and improves enzyme levels |
| Medications (Statins, Painkillers) | Talk to your doctor—don’t stop on your own. Ask about safer alternatives | Some drugs may elevate liver enzymes; your doctor can adjust them |
| Alcohol Use | Avoid all alcohol—even small amounts can be harmful | Alcohol stresses liver cells and significantly raises SGPT/SGOT |
| Viral Hepatitis (B/C) | Get tested for HBV/HCV. Start antiviral treatment if needed | Antivirals can lower liver inflammation and normalize enzymes |
These lifestyle interventions align with liver health protocols from DHA, SEHA, and MOHAP (UAE 2025). Always consult your doctor for personalized treatment.
Preparing for SGOT and SGPT Tests – Patient Checklist
To ensure accurate results, certain precautions and preparations are recommended before undergoing SGOT and SGPT testing. These enzyme tests are usually part of a comprehensive liver function panel, and the reliability of the results depends on adherence to pre-test guidelines.
Fasting may be required, especially if the tests are performed as part of a full liver panel that includes lipid profiles or glucose levels. Patients are generally advised to avoid eating or drinking anything other than water for 8–12 hours prior to the test, unless otherwise instructed by their healthcare provider.
It is also recommended to refrain from alcohol consumption and avoid strenuous physical activity for at least 24 hours before the test. Both alcohol and muscle exertion can temporarily elevate liver enzymes, potentially leading to misleading or falsely elevated results.
Patients should inform their doctor of all current medications and supplements, including over-the-counter drugs and herbal products. Certain medications—such as statins, anti-epileptics, antibiotics, and nonsteroidal anti-inflammatory drugs (NSAIDs)—can influence liver enzyme levels or interact with liver function.
By following these guidelines, patients can help ensure the most accurate representation of their liver enzyme activity, allowing for more reliable diagnosis and clinical decision-making.
Interpreting SGOT and SGPT Results with Other Liver Markers
While SGOT (AST) and SGPT (ALT) are key indicators of hepatocellular injury, their diagnostic value is significantly enhanced when interpreted alongside other liver function markers. A multi-marker approach offers a more complete view of liver health and helps differentiate between various types and stages of liver disease.
Bilirubin, a byproduct of red blood cell breakdown, is a critical marker for hepatic excretory function. Elevated bilirubin levels may indicate impaired bile flow, liver dysfunction, or hemolysis, especially when coupled with raised transaminase levels.
Alkaline phosphatase (ALP) and gamma-glutamyl transferase (GGT) are enzymes associated with the biliary tract. Their elevation often points to cholestatic or obstructive liver disease, such as gallstones, bile duct strictures, or primary biliary cirrhosis. When ALP and GGT levels rise alongside SGOT and SGPT, a mixed hepatocellular-cholestatic pattern is suspected.
International Normalized Ratio (INR), a measure of blood clotting function, indirectly reflects the liver’s synthetic ability. A prolonged INR, especially in combination with elevated liver enzymes and bilirubin, may indicate advanced liver dysfunction or hepatic failure.
Combining these markers provides a comprehensive hepatic profile, allowing clinicians to better assess the extent, nature, and urgency of liver damage. It also supports differential diagnosis and informs the need for further imaging, biopsy, or specialist consultation.
Interpretation Matrix for SGOT and SGPT Levels
Understanding whether your liver enzyme levels fall within the normal, mildly elevated, or severely elevated range can help pinpoint the underlying cause. The matrix below breaks down SGOT (AST) and SGPT (ALT) values and maps them to possible liver and non-liver conditions for accurate clinical interpretation.
| Enzyme | Normal Range | Mild Elevation (1–2x) |
Moderate Elevation (2–5x) |
Severe Elevation (>5x) |
Possible Clinical Causes |
|---|---|---|---|---|---|
| SGPT (ALT) | 7–56 U/L | Up to ~112 U/L | ~112–280 U/L | >280 U/L |
|
| SGOT (AST) | 5–40 U/L | Up to ~80 U/L | ~80–200 U/L | >200 U/L |
|
Is High SGPT/SGOT Dangerous? When to See a Liver Specialist
High SGPT and SGOT levels are dangerous when they stay elevated for more than 12 weeks, rise above 5× the normal limit, or are combined with symptoms like jaundice, fatigue, or abnormal ultrasound findings. If your liver enzymes remain high despite lifestyle changes or show a De Ritis ratio >2:1 (suggestive of alcoholic liver damage), you should see a hepatologist. In the UAE, DHA and SEHA recommend specialist referral when enzymes exceed 3× normal and imaging or lab findings suggest fibrosis or liver inflammation.
Persistent or significantly elevated SGPT and SGOT levels may indicate progressive liver injury. The following risk-based matrix helps determine when enzyme levels require further monitoring versus immediate specialist referral in the UAE healthcare system.
| SGPT/SGOT Level | Risk Level | Possible Causes | Action Required | Referral Trigger (UAE Protocol) |
|---|---|---|---|---|
| <2× ULN | Low | Minor DILI, NAFLD, transient stress, alcohol, exercise | Reassess in 4–6 weeks, address reversible factors | Not required unless recurrence or symptoms |
| 2–5× ULN | Moderate | NAFLD, NASH, viral hepatitis, medication toxicity | Order LFT repeat, hepatobiliary ultrasound, initiate viral/autoimmune screening | Refer if persistent elevation ≥12 weeks |
| >5× ULN | High | Acute viral hepatitis, ischemic liver injury, severe DILI | Urgent full workup including coagulation panel, FibroScan, immunologic markers | Mandatory referral to DHA/SEHA hepatology |
| AST:ALT >2:1 | Diagnostic Alert | Alcoholic hepatitis, advanced fibrosis | Recommend alcohol cessation, micronutrient therapy, inpatient management if symptomatic | Yes — refer with Maddrey scoring |
| SGPT/SGOT + ↑ INR, ↓ albumin | Decompensated Liver | Cirrhosis, hepatic failure | Tertiary care admission; screen for encephalopathy, ascites, varices | Emergency referral per MOHAP/DHA protocols |
Glossary for SGOT and SGPT Testing in UAE
To better understand your liver enzyme reports and navigate testing options in the UAE, it’s important to grasp the terminology used in diagnostics. The glossary below breaks down essential clinical abbreviations, liver-related conditions, and institutional acronyms you may encounter during SGOT/SGPT testing or follow-up care.
| Term | Full Form | Clinical Role / Diagnostic Use | Related Concepts |
|---|---|---|---|
| ALT (SGPT) | Alanine Aminotransferase | Liver-specific enzyme; elevated in hepatocellular injury (e.g., NAFLD, hepatitis) | AST, De Ritis Ratio, NAFLD |
| AST (SGOT) | Aspartate Aminotransferase | Found in liver, heart, muscle; elevation may indicate liver or non-hepatic injury | ALT, MI, Muscle Trauma |
| De Ritis Ratio | AST/ALT Ratio | Helps differentiate alcoholic vs. non-alcoholic liver damage | Alcoholic Hepatitis, NASH |
| NAFLD | Non-Alcoholic Fatty Liver Disease | Fat accumulation in liver without alcohol use; common ALT cause | Metabolic Syndrome, NASH |
| NASH | Non-Alcoholic Steatohepatitis | Progressive NAFLD with inflammation and fibrosis | ALT, Fibrosis, FIB-4 Score |
| FibroScan | Transient Elastography | Non-invasive imaging test to assess liver stiffness and fibrosis | NASH, Cirrhosis |
| FIB-4 Score | Fibrosis-4 Index | Blood test algorithm for liver fibrosis staging | Platelets, ALT, AST |
| DHA | Dubai Health Authority | Regulatory body overseeing liver test protocols in Dubai | SEHA, MOHAP |
| SEHA | Abu Dhabi Health Services Company | Governs public hospital diagnostics across Abu Dhabi | OSHAD-SF, Visa Medical |
| MOHAP | Ministry of Health & Prevention | Federal UAE body for health regulation and licensing | DHA, SEHA, Test Mandates |
Conclusion
SGOT (AST) and SGPT (ALT) testing remains an indispensable component of liver health assessment in 2025—especially in regulated healthcare systems like the UAE and India. These enzymes serve as reliable indicators of hepatocellular injury and are widely used for diagnosing liver diseases, monitoring treatment response, and guiding further diagnostic decisions.
Understanding the pattern, ratio, and degree of enzyme elevation—alongside markers like bilirubin, ALP, GGT, and INR—enables clinicians to identify the root cause of liver dysfunction more accurately. From routine screenings to specialized hepatology referrals, SGOT and SGPT tests form the diagnostic foundation of evidence-based liver care.
Whether you’re a patient seeking early answers or a healthcare provider managing complex cases, timely and accurate interpretation of transaminase levels can lead to faster intervention, better outcomes, and more personalized treatment strategies.
FAQs – SGOT and SGPT Testing (2025)
Below are evidence-based answers to the most common patient queries about SGOT (AST) and SGPT (ALT) testing—covering diagnostic meanings, danger levels, test preparation, and lifestyle corrections.
What does a high SGPT mean?
An elevated SGPT (ALT) level reflects hepatocellular injury—typically from fatty liver disease, viral hepatitis, or drug toxicity. SGPT is liver-specific, making it a precise early indicator of inflammation within hepatic cells. Persistently high ALT may require ultrasound or FibroScan for deeper evaluation, especially in patients with metabolic risk factors like obesity or diabetes.
Do I need to fast before SGPT and SGOT tests?
Fasting is not required when SGPT/SGOT is tested alone. However, if your doctor has ordered a full liver panel or lipid profile, a fast of 8–12 hours may be recommended. Always follow the instructions given by your lab or physician. UAE diagnostic providers like Redcliffe Labs or Aster Clinics usually mention this during booking.
Which foods help reduce SGPT levels naturally?
Foods that support liver enzyme balance include:
- Leafy greens (spinach, kale)
- Broccoli, cauliflower (cruciferous veggies)
- Garlic, turmeric, green tea
- Omega-3 fish (salmon, sardines)
- Cold-pressed olive oil
Avoid: processed sugar, deep-fried food, and alcohol. These nutrition strategies are particularly effective in cases of NAFLD and NASH, as outlined in DHA/SEHA clinical nutrition protocols.
Are SGOT and SGPT included in routine blood tests?
Yes. SGOT (AST) and SGPT (ALT) are routinely included in Liver Function Test (LFT) panels. These are typically required for:
- Annual health checkups
- Visa medicals (as mandated by MOHAP)
- Pre-surgery assessments
- Occupational screenings like OSHAD-SF in Abu Dhabi
What’s the difference between SGOT and SGPT?
- SGPT (ALT) is more liver-specific and rises in most forms of liver cell damage.
- SGOT (AST) is found in liver and other tissues (heart, muscle, kidneys). It can elevate due to non-liver conditions like a heart attack or intense workout.
For deeper insight, doctors often use the AST/ALT ratio (De Ritis ratio) to differentiate alcoholic vs. metabolic liver disorders.
Can medications raise SGPT or SGOT levels?
Yes. The following drugs may cause liver enzyme elevations:
- Statins (cholesterol)
- Paracetamol (acetaminophen)
- NSAIDs (ibuprofen, diclofenac)
- Antibiotics (e.g., isoniazid)
- Anti-seizure medications (valproate, phenytoin)
Always report all medications to your healthcare provider before testing.
What lifestyle changes help lower SGPT levels?
To normalize SGPT:
- Exercise 30–45 minutes daily
- Follow a plant-based, low-sugar diet
- Maintain ideal body weight
- Eliminate alcohol
- Control blood sugar and cholesterol
In the UAE, personalized liver care plans are offered by Aster, Zulekha, LLH, and SEHA hepatology clinics.
Where can I get reliable SGOT/SGPT testing in the UAE or India?
UAE options:
- DHA-approved labs in Dubai (Aster, Zia)
- SEHA hospitals in Abu Dhabi (LLH, Burjeel, Medeor)
- Prices range from AED 89 to AED 220
India options:
- NABL-accredited labs like Metropolis, Dr. Lal PathLabs, Apollo Diagnostics
- Home sample collection is widely available
Can high SGPT or SGOT levels be reversed?
Yes. Reversal is often possible with:
- Weight loss (5–10% for NAFLD)
- Alcohol avoidance
- Liver-protective diet
- Controlled medication use
- Consistent physical activity
Repeat testing and lifestyle follow-through usually show normalization within 3–6 months in early-stage cases.
Can medications affect SGPT and SGOT levels
Yes. The following drugs may cause liver enzyme elevations:
- Statins (cholesterol)
- Paracetamol (acetaminophen)
- NSAIDs (ibuprofen, diclofenac)
- Antibiotics (e.g., isoniazid)
- Anti-seizure medications (valproate, phenytoin)
Always report all medications to your healthcare provider before testing.
How often should I get SGOT and SGPT levels checked?
If you’re at risk (NAFLD, diabetes, on hepatotoxic drugs), test every 3 to 6 months. For healthy individuals, annual testing during wellness screenings is sufficient.
Dr. Aisha Rahman is a board-certified internal medicine specialist with over 12 years of clinical experience in chronic disease management and preventive healthcare. She has worked at leading hospitals across the UAE, helping patients manage conditions such as diabetes, hypertension, cardiovascular diseases, and metabolic disorders.
A strong advocate for preventive medicine, Dr. Rahman emphasizes early diagnosis, lifestyle modifications, and patient education to reduce chronic illness risks. She is an active member of the Emirates Medical Association and has contributed to health awareness programs and medical research initiatives. Her expertise has been featured in The National UAE, Gulf Health Magazine, and leading medical journals. As a keynote speaker at healthcare conferences, she shares insights on evidence-based treatments, patient-centered care, and advancements in internal medicine.
Dr. Omar Al-Farsi is a clinical nutritionist and medical researcher with over 15 years of experience in dietary science, metabolic disorders, and preventive healthcare. He has served as a senior consultant for UAE healthcare authorities and contributed to public health initiatives focused on nutrition education and disease prevention.
Dr. Al-Farsi has collaborated with leading hospitals, research institutions, and universities in the UAE, ensuring that health information is scientifically accurate and evidence-based. His research has been published in Gulf Medical Journal, Dubai Health Review, and WHO Nutrition Reports, making significant contributions to nutrition science and public health awareness.