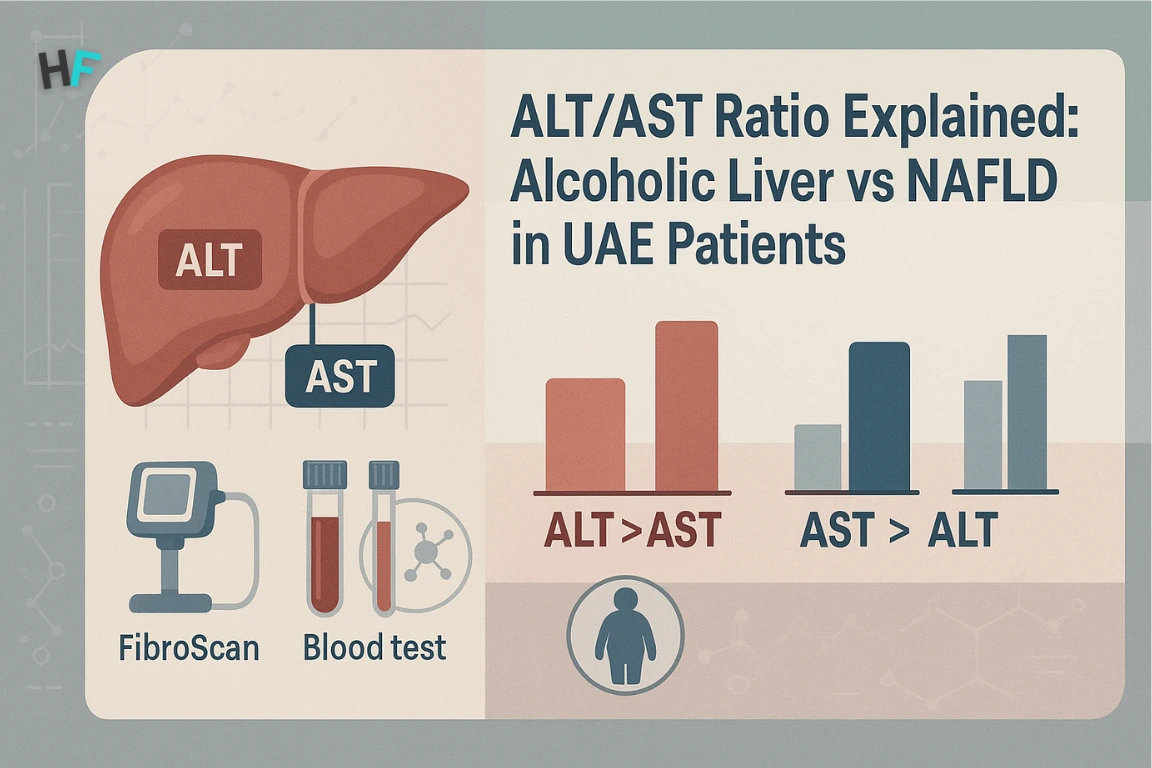
In 2025, the ALT/AST ratio has become a critical liver diagnostic marker in UAE healthcare, especially for distinguishing between alcoholic liver disease and non-alcoholic fatty liver disease (NAFLD). This ratio compares the levels of two enzymes—alanine aminotransferase (ALT), which is more specific to liver tissue, and aspartate aminotransferase (AST), which is found in both liver and muscle.
To understand how these enzymes are measured and interpreted in liver function tests, read our detailed guide on SGOT and SGPT tests in UAE.
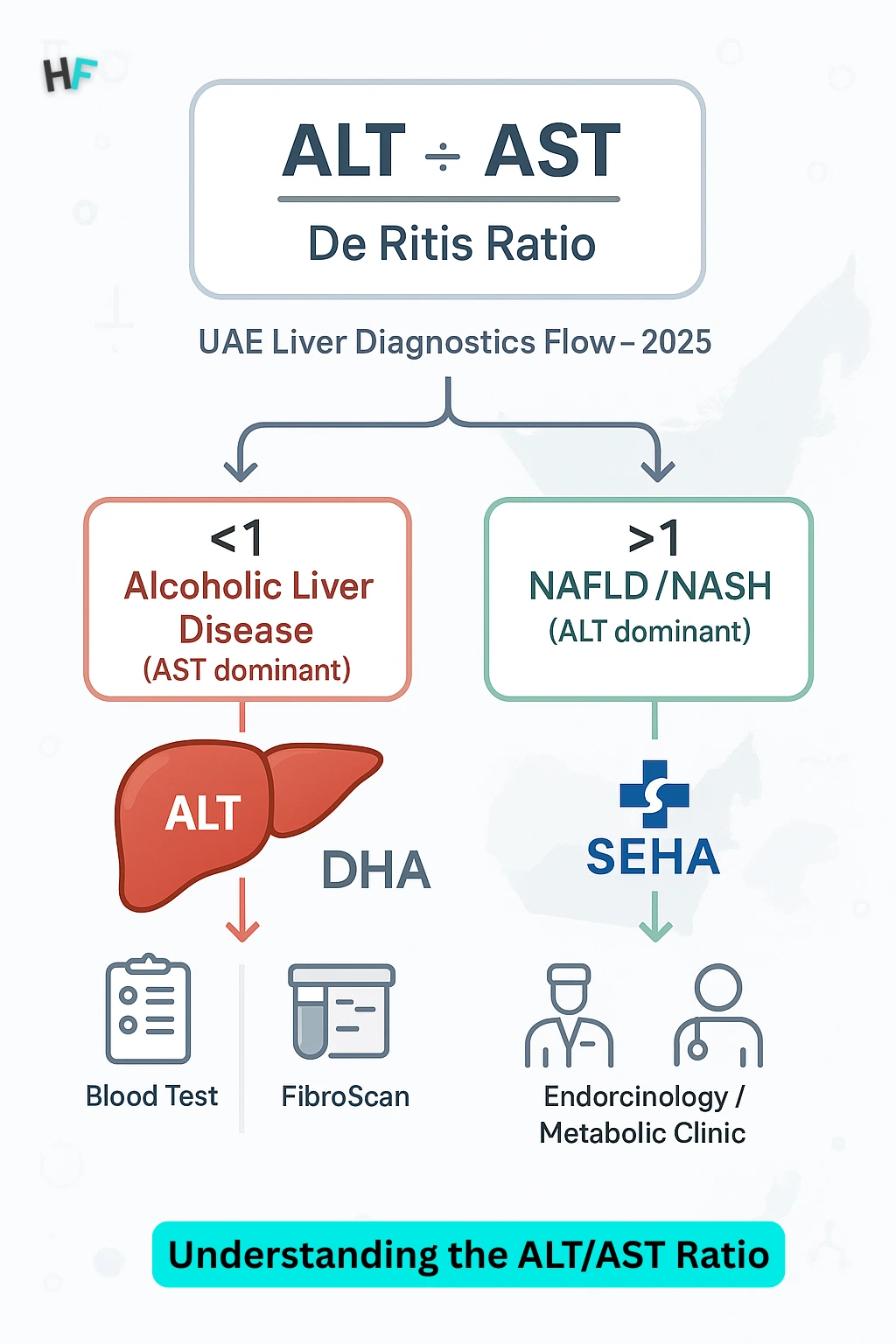
A ratio greater than 2:1 typically indicates alcohol-related liver damage such as alcoholic steatohepatitis, while a ratio below 1 usually suggests metabolic liver conditions like NAFLD or its more severe form, non-alcoholic steatohepatitis (NASH). Physicians across Dubai Health Authority (DHA) and SEHA facilities routinely use the ALT/AST ratio during preclinical screenings and liver consultations to guide diagnostic and referral decisions.
In a region facing rising metabolic syndrome and lifestyle-driven liver disease, early interpretation of ALT and AST levels helps clinicians determine whether to refer patients for alcohol-use evaluation, fibrosis staging via FibroScan, or metabolic risk profiling and lifestyle interventions—making this ratio a frontline tool in liver health management.
According to a 2023 study published in the Journal of Hepatology, NAFLD affects approximately 32% of adults in the Middle East, with UAE prevalence expected to rise significantly. Projections by GlobalData Healthcare estimate that by 2030, the number of NAFLD cases in the UAE could exceed 372,000, reinforcing the importance of early, enzyme-based liver disease differentiation.
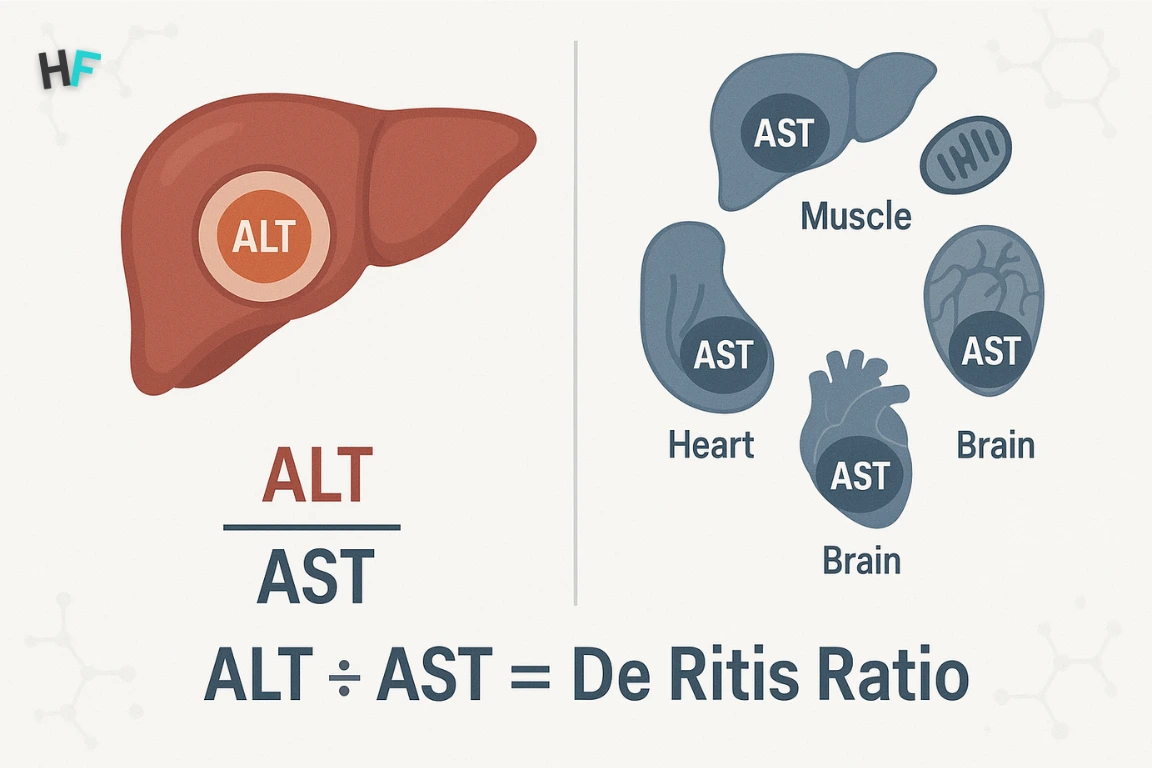
What Is the ALT/AST (De Ritis) Ratio?
The ALT/AST ratio—also known as the De Ritis ratio—is a valuable clinical marker used to interpret liver enzyme profiles. It compares alanine aminotransferase (ALT) to aspartate aminotransferase (AST):
ALT ÷ AST
ALT is primarily localized in the cytosol of hepatocytes, making it highly specific to liver cell injury. By contrast, AST is distributed across both the cytosol and mitochondria and is present in various tissues, including skeletal muscle, cardiac muscle, and the brain—which makes it less liver-specific and more reflective of multisystemic damage.
How is the ALT/AST ratio used in UAE healthcare?
In 2025 UAE clinical settings, particularly within DHA and SEHA facilities, the ALT/AST ratio is routinely assessed as part of liver function testing. These enzymes are also covered in depth in our SGOT/SGPT enzyme analysis guide, which outlines typical reference ranges and clinical relevance. This ratio provides essential diagnostic insights into the underlying cause of enzyme elevation:
ALT/AST ratio <1 is often observed in alcoholic liver disease (ALD), particularly in alcoholic steatohepatitis (ASH), due to mitochondrial AST release.
Given the growing burden of both metabolic syndrome and alcohol-related liver disorders in the UAE, the De Ritis ratio plays a central role in differentiating between these conditions. It informs downstream diagnostic strategies such as FibroScan® for non-invasive fibrosis staging and guides referrals to hepatology or endocrinology specialists based on the suspected cause.
By integrating enzyme ratios into routine screenings, UAE clinicians can better triage patients, ensure timely interventions, and deliver more personalized liver care—whether in public hospitals or private specialty centers.
Understanding the ALT/AST Ratio: Clinical Meaning & Thresholds
The ALT/AST ratio (De Ritis ratio) is a clinically validated tool for identifying the source and severity of liver injury. It compares alanine aminotransferase (ALT) to aspartate aminotransferase (AST) and guides differential diagnosis between alcoholic liver disease, non-alcoholic fatty liver disease (NAFLD), non-alcoholic steatohepatitis (NASH), and viral hepatitis.
In UAE healthcare systems—especially within DHA and SEHA workflows—the ALT/AST ratio supports early triage, hepatology referral, and further diagnostic evaluation.
ALT/AST Ratio Thresholds and Clinical Interpretation
The table below summarizes how specific ALT/AST ratio thresholds correlate with underlying liver pathology, helping clinicians differentiate between alcohol-induced and metabolic liver injuries.
| ALT/AST Ratio | Interpretation | Common Causes |
|---|---|---|
| < 1.0 | AST > ALT → Mitochondrial-dominant injury | Alcoholic hepatitis, cirrhosis |
| ≈ 1.0 | ALT ≈ AST → Non-specific elevation | Early liver injury, mild hepatopathy |
| > 1.2 | ALT > AST → Cytosolic-dominant leakage | NAFLD, NASH, viral hepatitis |
Clinical Notes:
- < 1.0: Elevated AST reflects mitochondrial injury. Seen in alcoholic hepatitis, fibrosis, or cirrhosis, where alcohol disrupts mitochondrial integrity.
- ≈ 1.0: Equal enzyme levels indicate a non-specific liver response. May reflect transient inflammation or early hepatocyte stress. Requires follow-up testing or metabolic screening.
- > 1.2: ALT predominance suggests cytosolic enzyme release. Typically linked to NAFLD, NASH, or viral hepatitis, especially in UAE populations with metabolic syndrome.
ALT/AST in NAFLD: Clinical Interpretation in UAE Patients
In non-alcoholic fatty liver disease (NAFLD), ALT is the dominant enzyme released due to its cytoplasmic localization within hepatocytes—where fat accumulation and metabolic stress trigger early liver injury. This ALT-dominant pattern also applies to non-alcoholic steatohepatitis (NASH), particularly in patients with obesity, insulin resistance, or type 2 diabetes.
ALT > AST: Pathophysiology in NAFLD
NAFLD arises from hepatic fat accumulation, often triggered by insulin resistance and chronic low-grade inflammation. These metabolic disruptions cause cytosolic stress and hepatocyte swelling, which primarily release ALT. While AST may be mildly elevated, it usually remains below ALT unless significant fibrosis or cirrhosis develops.
An ALT/AST ratio above 1.2 often signals ongoing hepatocellular inflammation, particularly in patients with metabolic syndrome or visceral obesity—two of the most common comorbidities in UAE clinical practice.
DHA/SEHA NAFLD Workflow: Enzyme Ratio to Diagnostic Action
In the UAE, DHA and SEHA healthcare facilities integrate ALT/AST interpretation into standard liver function screening protocols. When the enzyme pattern suggests NAFLD, clinicians follow a structured evaluation process:
- Metabolic Risk Profiling: Fasting glucose, HbA1c, lipid panel, waist circumference, and blood pressure.
- Liver Imaging: Ultrasound, MRI-PDFF, or FibroScan (transient elastography) to quantify steatosis and rule out fibrosis.
Referral for Lifestyle and Endocrine Management: Based on severity, patients may be referred to a dietician, endocrinologist, or bariatric specialist for structured intervention.
This enzyme-driven workflow ensures early detection of metabolic liver disease, even in patients without overt symptoms.
These patterns align with what’s seen in SGPT/SGOT trends, as detailed in our UAE-based liver enzyme interpretation article.
Do we have regional data supporting ALT/AST usage in NAFLD?
While UAE-specific data on ALT/AST ratio thresholds in NAFLD remain limited, international studies consistently report that ALT levels tend to exceed AST in metabolic liver disease—especially in patients with obesity, type 2 diabetes, or dyslipidemia. Regional data from Gulf countries, including Saudi Arabia and Qatar, reflect similar metabolic profiles, supporting the presence of NAFLD in non-drinking populations with elevated ALT.
Although formal ratio-based cutoff studies (>1.2) are sparse in the region, these findings underscore the clinical utility of ALT-dominant enzyme patterns as an early signal for steatotic liver injury in UAE patient populations.
ALT/AST in NAFLD & NASH: The UAE Epidemic
In the UAE, non-alcoholic fatty liver disease (NAFLD) is increasing due to high rates of obesity, physical inactivity, and type 2 diabetes. In metabolic liver conditions like NAFLD or non-alcoholic steatohepatitis (NASH), ALT levels are higher than AST, which signals damage to the liver cell cytoplasm. When the ALT/AST ratio exceeds 1.2, it serves as an early red flag for progressive liver inflammation. DHA and SEHA clinicians use this ratio to trigger additional metabolic and imaging assessments.
A 2023 meta-analysis published in the Journal of Hepatology estimated that non-alcoholic fatty liver disease (NAFLD) affects approximately 42.6% of adults in the Middle East and North Africa (MENA), including populations in the UAE. Additionally, modeling studies by GlobalData Healthcare project that NAFLD cases in the UAE could exceed 372,000 by 2030, driven by rising obesity, insulin resistance, and sedentary lifestyle patterns. During DHA and SEHA liver function screenings, an ALT/AST ratio above 1.2 prompts evaluation of metabolic risk markers, such as fasting glucose, HbA1c, lipid profiles, and non-invasive imaging including ultrasound or MRI-PDFF (proton density fat fraction), to assess hepatic fat accumulation.
Limitations of the ALT/AST Ratio: What It Cannot Tell You
While the ALT/AST ratio is a useful initial marker for differentiating liver disease types, it has important diagnostic limitations. Most critically, it is not a fibrosis staging tool. A normal or altered ratio cannot determine the degree of liver scarring—which must be assessed through elastography (FibroScan) or, in some cases, liver biopsy. According to DHA clinical guidelines, FibroScan is recommended for UAE patients with persistent enzyme elevation, fatty liver on imaging, or abnormal ratios without a clear cause.
The ALT/AST ratio can also be skewed by non-hepatic factors. Common medications like paracetamol, statins, and certain antibiotics can temporarily elevate liver enzymes without indicating chronic liver disease. Viral load, herbal supplements, and autoimmune flares may also distort transaminase levels.
Patient-specific variables—including age, gender, and ethnic background—further influence ALT/AST baselines. In the UAE’s diverse population, interpretation requires context from a complete liver panel (bilirubin, ALP, GGT, albumin) along with imaging data to form a reliable diagnosis and staging profile.
When to Consult a Liver Specialist in the UAE?
You should consult a liver specialist in the UAE if your ALT/AST ratio is consistently abnormal or if liver enzyme levels remain elevated for more than six weeks. These patterns can signal early-stage liver damage, alcoholic hepatitis, or metabolic steatohepatitis (NASH), all of which require expert evaluation.
In both DHA and SEHA healthcare settings, abnormal ALT/AST findings trigger a standard referral workflow that includes non-invasive imaging such as FibroScan or abdominal ultrasound. This helps determine the extent of fibrosis, fat accumulation, or inflammation. A ratio above 2:1, or ALT elevations without a known cause, should not be ignored—especially in patients with diabetes, obesity, or regular alcohol use.
Need to Speak with a Liver Specialist in Dubai or Abu Dhabi?
Early evaluation can prevent irreversible liver damage. If you’re in Dubai, Abu Dhabi, or Sharjah, schedule a consultation with a board-certified hepatologist.
👉 Find a liver specialist in Dubai
FAQs on ALT/AST Ratio
Patients often have specific questions about how the ALT/AST ratio works, what the numbers mean, and when it signals something serious. Below are concise answers to the most frequently searched ALT/AST questions in UAE clinical contexts.
What does a high ALT/AST ratio mean?
A high ALT/AST ratio—typically greater than 1.2—suggests non-alcoholic fatty liver disease (NAFLD) or non-alcoholic steatohepatitis (NASH), particularly in patients with metabolic risk factors like obesity or diabetes.
Can I calculate the ALT/AST ratio at home?
Yes, you can calculate it using recent lab test values. Simply divide your ALT level by your AST level (ALT ÷ AST). However, interpretation should always be done by a clinician within the context of a full liver panel and clinical history.
Does fasting affect the ALT/AST ratio?
Fasting has minimal effect on ALT or AST levels in healthy individuals. However, extreme fasting or malnutrition can occasionally alter liver enzyme dynamics, especially in metabolic syndrome cases.
Why is AST higher than ALT in alcoholics?
In alcohol-related liver disease, AST is often elevated more than ALT, typically in a 2:1 ratio, due to mitochondrial damage and vitamin B6 deficiency, which suppresses ALT production.
What if both ALT and AST are normal but the ratio is high?
If both enzymes are within normal range but the ratio is elevated, it may still indicate a subclinical or early liver condition, or a non-hepatic influence (e.g., muscle injury). Further evaluation with FibroScan or metabolic testing is advised.
Dr. Aisha Rahman is a board-certified internal medicine specialist with over 12 years of clinical experience in chronic disease management and preventive healthcare. She has worked at leading hospitals across the UAE, helping patients manage conditions such as diabetes, hypertension, cardiovascular diseases, and metabolic disorders.
A strong advocate for preventive medicine, Dr. Rahman emphasizes early diagnosis, lifestyle modifications, and patient education to reduce chronic illness risks. She is an active member of the Emirates Medical Association and has contributed to health awareness programs and medical research initiatives. Her expertise has been featured in The National UAE, Gulf Health Magazine, and leading medical journals. As a keynote speaker at healthcare conferences, she shares insights on evidence-based treatments, patient-centered care, and advancements in internal medicine.
Dr. Omar Al-Farsi is a clinical nutritionist and medical researcher with over 15 years of experience in dietary science, metabolic disorders, and preventive healthcare. He has served as a senior consultant for UAE healthcare authorities and contributed to public health initiatives focused on nutrition education and disease prevention.
Dr. Al-Farsi has collaborated with leading hospitals, research institutions, and universities in the UAE, ensuring that health information is scientifically accurate and evidence-based. His research has been published in Gulf Medical Journal, Dubai Health Review, and WHO Nutrition Reports, making significant contributions to nutrition science and public health awareness.