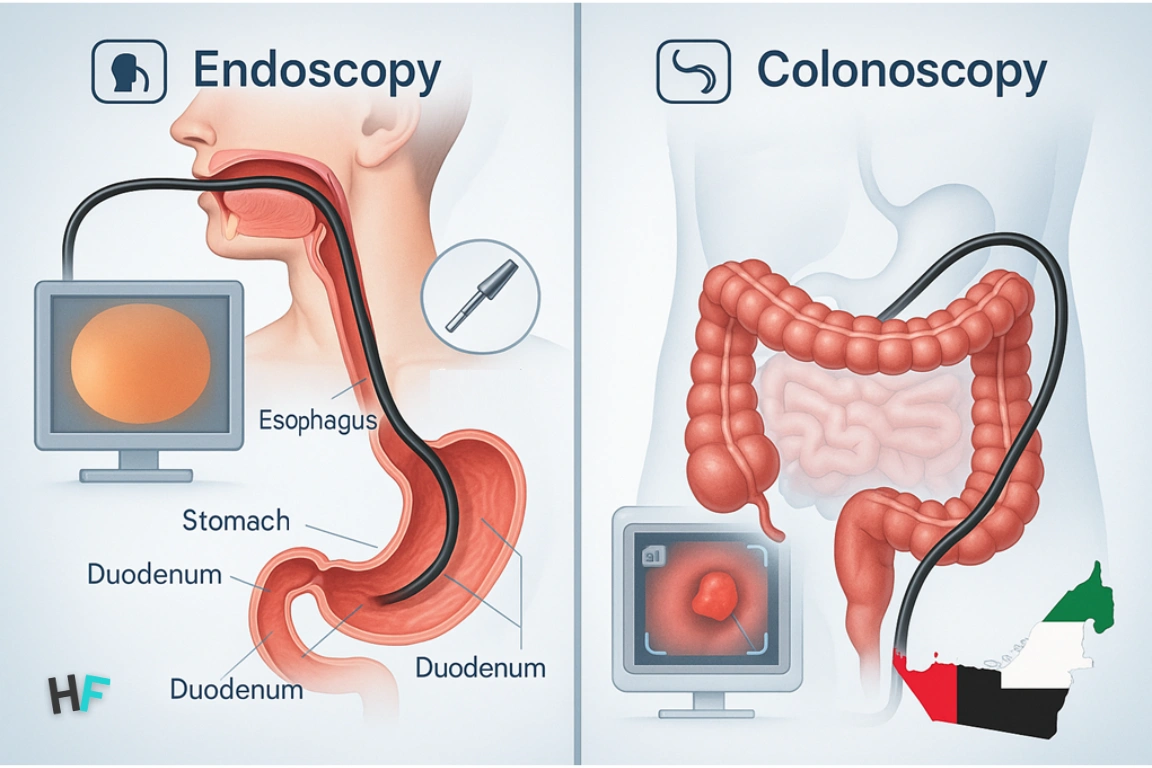
Endoscopy and colonoscopy are the two most commonly used procedures to examine the digestive system. Both involve inserting a flexible tube with a camera, but they target different parts of the gastrointestinal tract and serve distinct purposes.
Endoscopy (gastroscopy) examines the esophagus, stomach, and duodenum—typically for symptoms like reflux or upper abdominal pain. Colonoscopy, in contrast, assesses the colon and rectum, mainly for colorectal cancer screening or chronic bowel issues.
In the UAE, these procedures are widely available in both public and private hospitals. The integration of AI-assisted diagnostics, high-definition imaging, and sedation protocols has improved accuracy and patient comfort.
These tools not only diagnose but also allow biopsy and treatment in the same session. Choosing the right procedure depends on the symptoms and location of concern—an area increasingly supported by clinical triage in UAE hospitals.
What is Endoscopy?
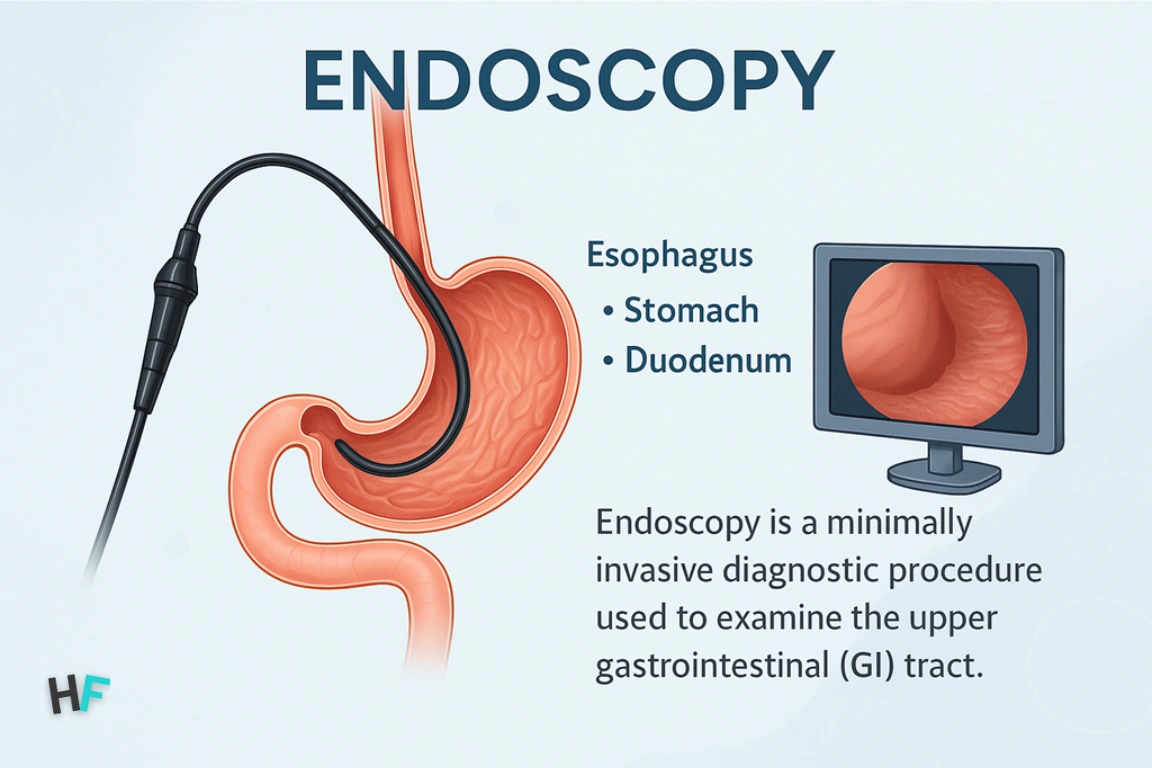
An endoscopy is a minimally invasive procedure that allows doctors to examine the upper digestive tract, including the esophagus, stomach, and duodenum. A flexible tube with a high-definition camera, called an endoscope, is inserted through the mouth to provide real-time imaging of the mucosal surfaces.
In the UAE, this procedure—often termed a gastroscopy—is commonly used to diagnose chronic heartburn, difficulty swallowing, persistent upper abdominal pain, or suspected ulcers. Hospitals like Cleveland Clinic Abu Dhabi and Mediclinic City Hospital use advanced Olympus EVIS EXERA III systems with narrow-band imaging (NBI), enabling early detection of gastric cancers and Barrett’s esophagus.
Unlike CT or ultrasound, endoscopy offers direct visualization and immediate biopsy, making it a core tool in modern gastroenterology. The procedure typically lasts 15–30 minutes, is done under conscious sedation, and allows for same-day discharge in most UAE clinics.
What is Colonoscopy?
A colonoscopy is an endoscopic procedure used to examine the colon and rectum. A flexible video colonoscope is inserted through the rectum, allowing real-time visualization of the large intestine and often the terminal ileum. The device can navigate intestinal curves, inflate the colon for clearer views, and remove tissue samples or polyps during the same session.
In the UAE, colonoscopy is routinely performed to:
- Screen for colorectal cancer (starting at age 45)
- Evaluate chronic constipation or diarrhea
- Monitor Inflammatory Bowel Disease (IBD)
- Investigate unexplained GI bleeding
UAE hospitals like Sheikh Shakhbout Medical City now use AI-powered polyp detection and CO₂ insufflation, improving visibility and patient comfort. The procedure takes 30–60 minutes and requires prior bowel prep using PEG-based solutions. Most patients are sedated and discharged the same day.
Because precancerous polyps can be removed immediately, colonoscopy remains the gold standard for both diagnosis and prevention of colorectal disease.
What is the difference between endoscopy and colonoscopy?
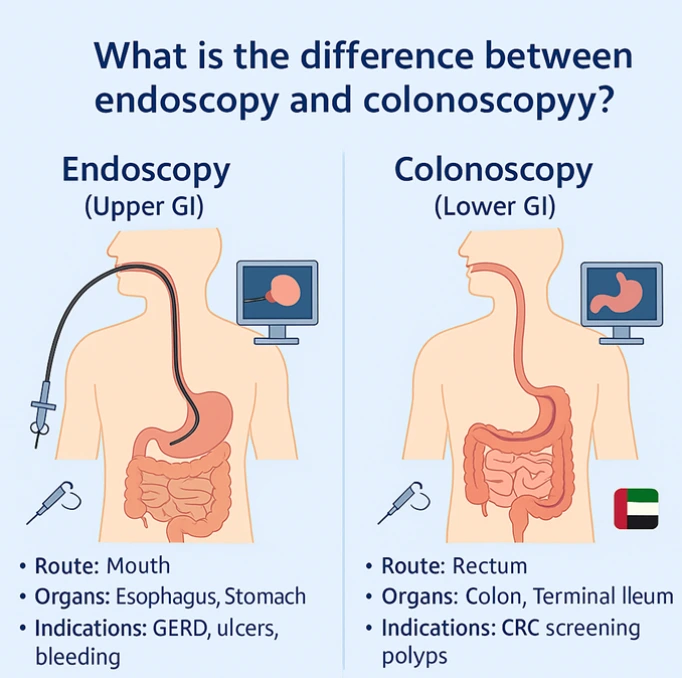
The key difference lies in the anatomical target, entry point, and purpose of each procedure. Both use flexible video scopes, but are designed for different sections of the gastrointestinal tract.
- Endoscopy (esophagogastroduodenoscopy or EGD) is used for the upper GI tract—esophagus, stomach, and duodenum. It’s performed by inserting a scope through the mouth.
- Colonoscopy examines the lower GI tract—colon and rectum—by inserting the scope through the anus.
In UAE hospitals, referral is symptom-guided:
- Upper GI symptoms (e.g., reflux, dysphagia, upper abdominal pain) → Endoscopy
- Lower GI symptoms (e.g., bleeding, bowel habit changes) → Colonoscopy
Diagnostic Comparison Table: Endoscopy vs Colonoscopy in UAE
| Parameter | Endoscopy (EGD) | Colonoscopy |
|---|---|---|
| Region Visualized | Esophagus, Stomach, Duodenum | Rectum, Colon, Terminal Ileum |
| Route of Insertion | Oral (through mouth) | Rectal (through anus) |
| Common UAE Indications | GERD, ulcers, H. pylori, upper GI bleeding | CRC screening, IBD, polyps |
| Preparation Required | Fasting (6–8 hrs) | Bowel cleansing (PEG solutions) |
| Procedure Duration | 15–30 minutes | 30–60 minutes |
| Sedation Type | Conscious sedation | Moderate to deep sedation |
| Biopsy & Therapeutics | Yes – ulcer biopsy, variceal banding | Yes – polyp removal, biopsy, bleeding control |
| Cancer Detection Role | Esophageal & Gastric Cancer | Colorectal Cancer (CRC) |
| Typical Equipment Used | Olympus EVIS, NBI scopes | AI-assisted scopes, CO₂ insufflation |
| Recovery Time | Same-day discharge | Post-anesthesia recovery (~1 hour) |
| Screening Role in UAE | Diagnostic (symptom-driven) | Preventive (routine CRC screening from age 45) |
Why are endoscopy and colonoscopy procedures important in gastrointestinal diagnostics?
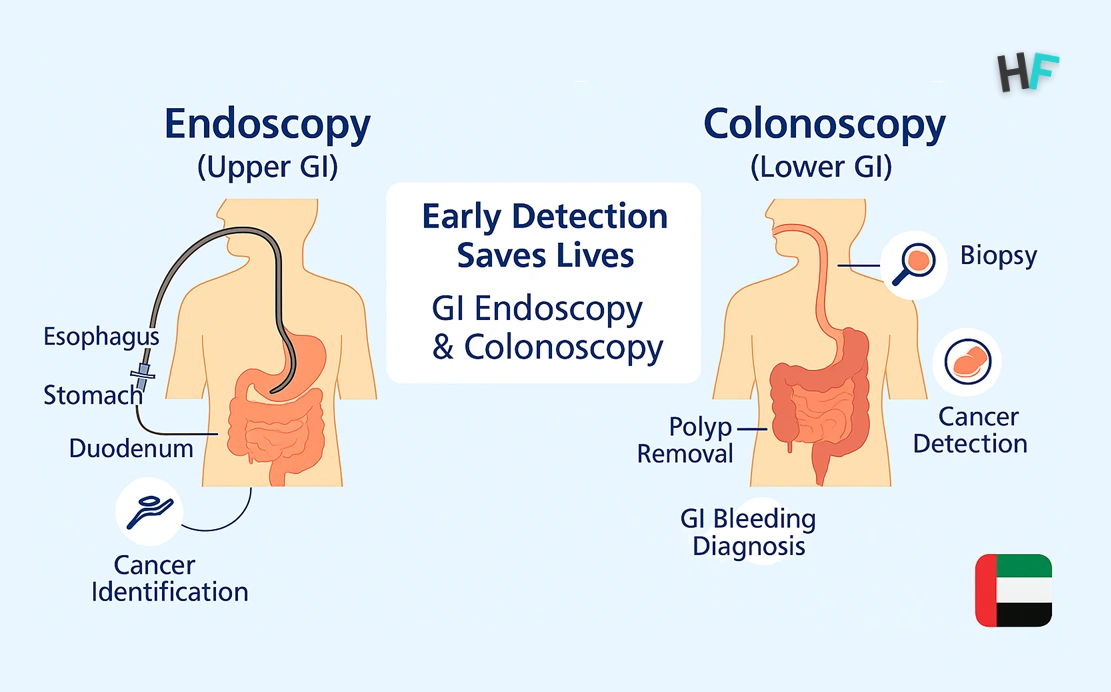
Endoscopy and colonoscopy are critical diagnostic tools in modern gastroenterology because they offer direct visualization of mucosal pathology, enable targeted tissue biopsy, and facilitate real-time therapeutic intervention. Unlike imaging modalities such as ultrasound or CT scans, these procedures allow clinicians to examine the actual internal linings of the digestive tract under magnification, assess vascular patterns, and capture tissue samples for histopathological evaluation.
In the UAE healthcare ecosystem, where gastrointestinal disorders like acid reflux, peptic ulcers, irritable bowel disease (IBD), and colorectal cancer (CRC) are increasingly prevalent, these procedures form the backbone of early detection, risk stratification, and treatment planning.
Key Diagnostic Roles of Endoscopy in UAE:
- GERD and Barrett’s Esophagus: Chronic reflux symptoms require endoscopy to evaluate for esophagitis and rule out premalignant metaplasia.
- Peptic Ulcer Disease: Active ulcers, bleeding points, or H. pylori-related mucosal damage can be directly visualized and biopsied.
- Gastric Cancer Risk: In high-risk populations (e.g., patients with persistent dyspepsia over age 40), gastroscopy is used for surveillance and biopsy.
- Upper GI Bleeding: Varices, Mallory-Weiss tears, and ulcers can be diagnosed and treated (e.g., banding, cauterization) during the same session.
Key Diagnostic Roles of Colonoscopy in UAE:
- Colorectal Cancer Screening: Colonoscopy is the gold standard for identifying adenomatous polyps and early-stage carcinomas.
- Chronic Diarrhea or Constipation: Allows exclusion of organic pathologies such as Crohn’s disease, ulcerative colitis, or ischemic colitis.
- Iron-Deficiency Anemia: In the absence of upper GI sources, colonoscopy is used to evaluate for occult bleeding from colon polyps or malignancies.
- Post-Polypectomy Surveillance: Repeat colonoscopies are performed based on polyp type, size, and dysplasia grade, as per UAE colorectal screening protocols.
Diagnostic Importance from a UAE Public Health Perspective
The Dubai Health Authority (DHA) and Department of Health – Abu Dhabi (DOH) promote early detection of GI diseases through structured endoscopic screening programs. These include:
- CRC screening starting at age 45 for asymptomatic adults
- Annual surveillance for patients with a family history of CRC or hereditary syndromes (e.g., Lynch Syndrome, FAP)
- Routine upper GI endoscopy for persistent dyspepsia, especially in high-risk expatriate populations from East Asia and South Asia
Because many GI conditions remain asymptomatic in early stages, these procedures enable intervention before clinical deterioration or malignant transformation.
Diagnostic vs. Therapeutic Integration
What makes endoscopy and colonoscopy uniquely valuable is their ability to transition instantly from diagnosis to intervention. For example:
- A bleeding gastric ulcer identified during endoscopy can be cauterized.
- A suspicious colon polyp found during colonoscopy can be excised and sent for histology.
- Strictures can be dilated, varices banded, and lesions tattooed—all without requiring a second procedure.
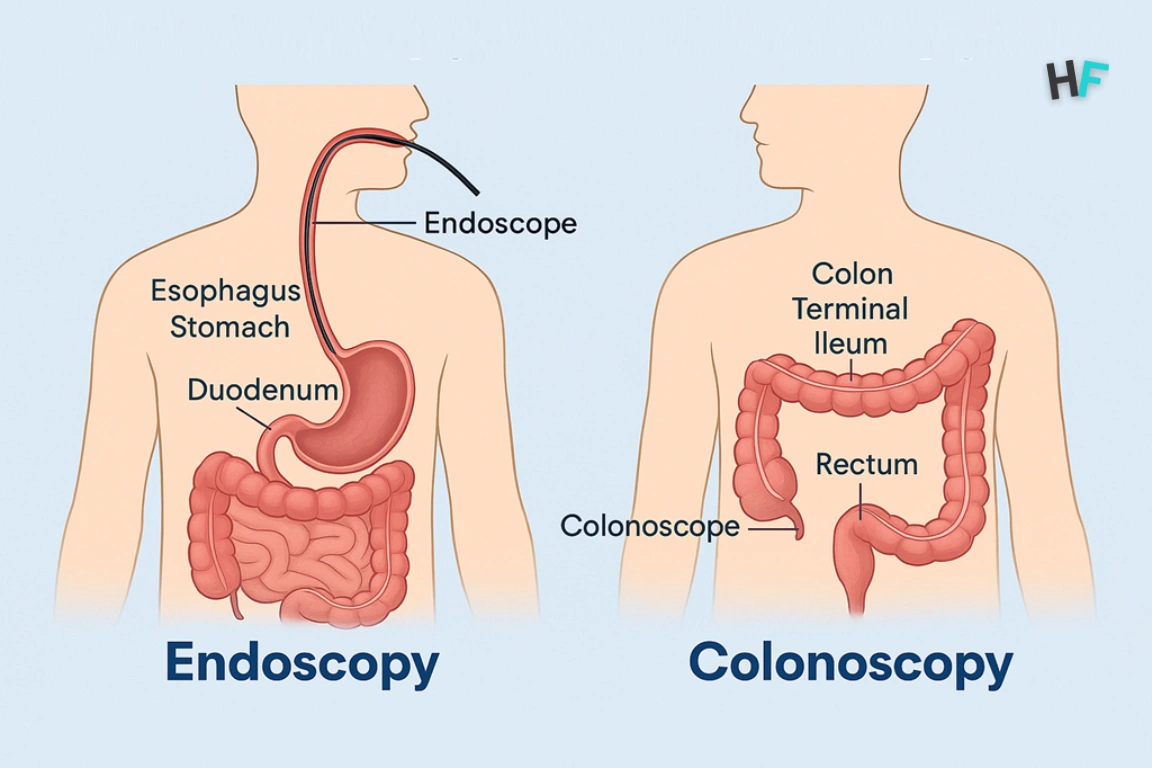
Which organs do endoscopy and colonoscopy examine?
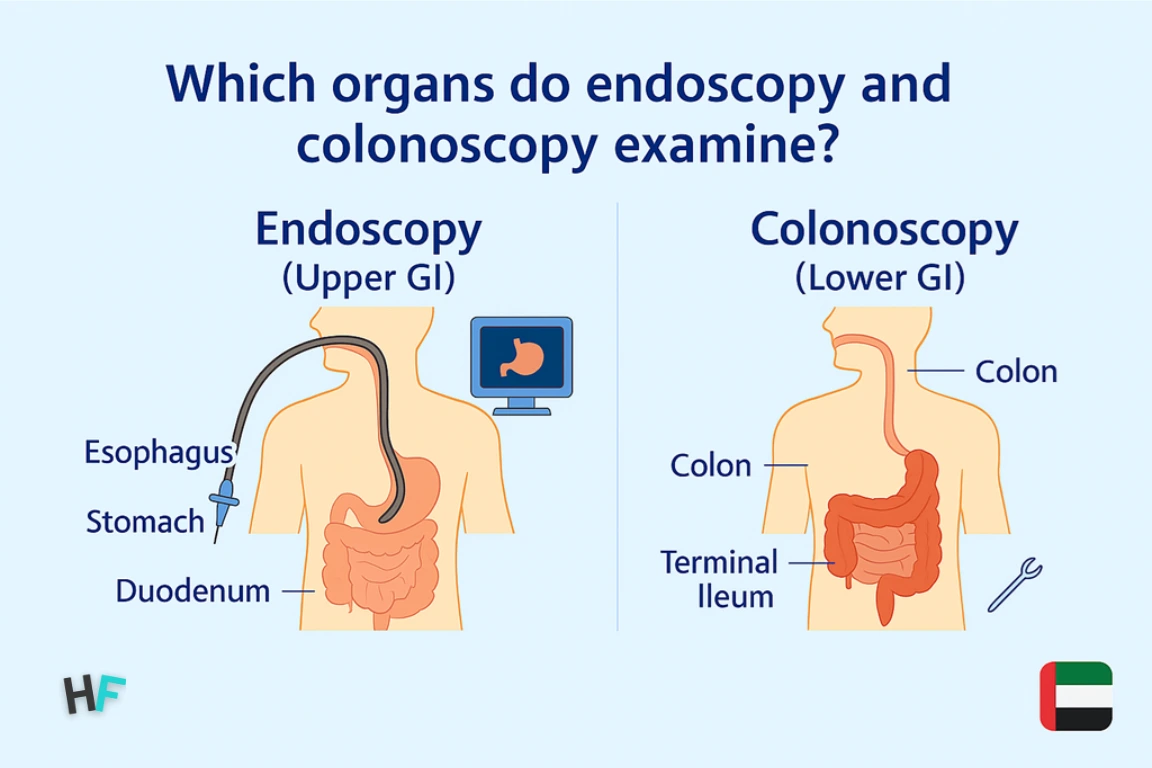
Endoscopy and colonoscopy differ primarily in the segment of the gastrointestinal tract they examine, with each targeting a distinct anatomical pathway based on clinical indication. Upper GI endoscopy, or gastroscopy, is performed via the mouth and allows direct visualization of the esophagus, stomach, and duodenum—the first part of the small intestine. This procedure is used to evaluate mucosal inflammation, ulcers, varices, strictures, and suspected upper GI malignancies.
In contrast, colonoscopy is introduced through the rectum and inspects the entire colon, including the rectum, sigmoid colon, descending, transverse, ascending colon, and cecum, with the option to intubate the terminal ileum when small bowel pathology is suspected. Colonoscopy enables assessment of colorectal polyps, mucosal irregularities, inflammatory bowel diseases, and occult bleeding sources. While the upper scope terminates at the duodenum, and the lower scope begins at the rectum, both procedures collectively map nearly the full length of the digestive tract, excluding much of the jejunum and ileum—areas accessible only by capsule endoscopy or enteroscopy in specific cases.
In UAE hospitals, this anatomical targeting is matched precisely to patient symptoms: heartburn, epigastric pain, or dysphagia typically necessitate gastroscopy; rectal bleeding, altered bowel habits, or family history of colorectal cancer trigger colonoscopic referral. Choosing the correct scope is not about preference—it’s a direct mapping of symptom location to internal anatomy, supported by years of clinical pattern recognition.
What Symptoms Indicate the Need for Endoscopy or Colonoscopy?
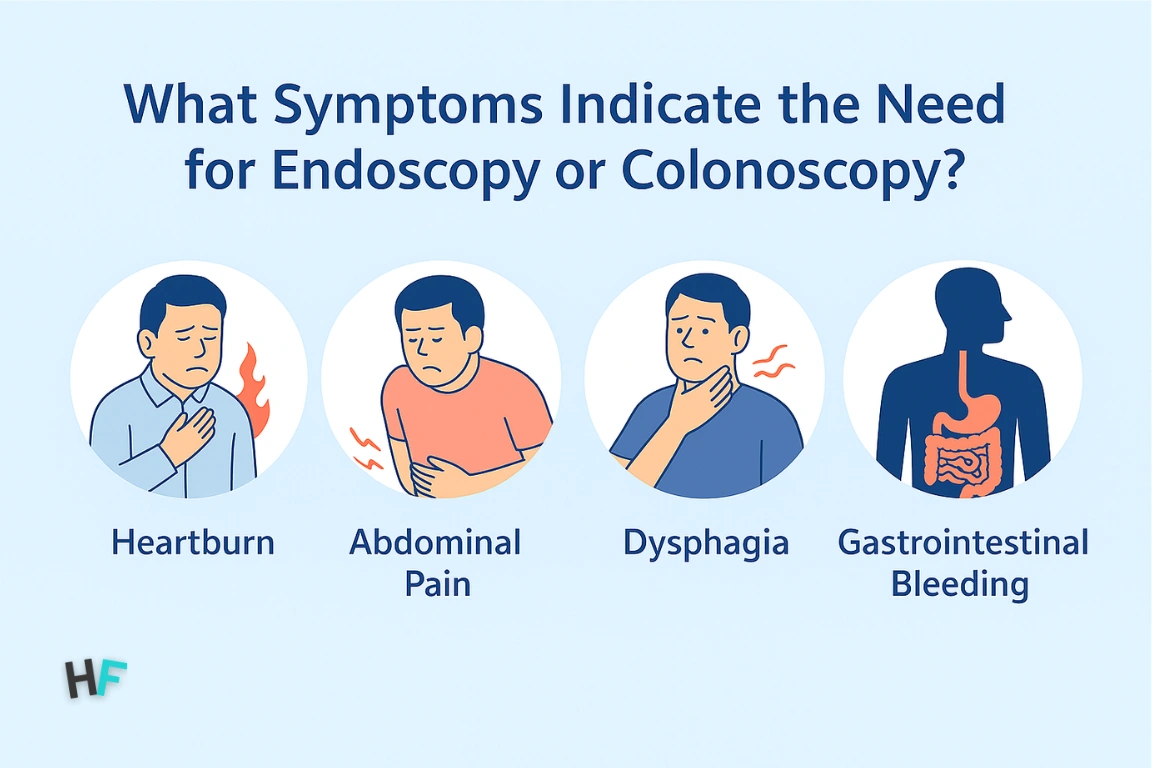
The choice between endoscopy and colonoscopy depends on where in the digestive tract symptoms occur—and how severe they are.
Endoscopy (Upper GI): Used when symptoms affect the esophagus, stomach, or duodenum.
- Persistent heartburn or reflux
- Upper abdominal pain
- Difficulty swallowing (dysphagia)
- Unexplained nausea or vomiting
- Early satiety or suspected ulcers
In the UAE, gastroscopy is routinely ordered for suspected H. pylori, ulcers, or chronic gastritis. When weight loss, anemia, or persistent vomiting is present, the urgency for endoscopy increases.
Colonoscopy (Lower GI): Ordered when symptoms suggest large bowel involvement.
- Rectal bleeding
- Chronic diarrhea or constipation
- Pencil-thin stools
- Bloating or iron-deficiency anemia
UAE hospitals follow referral pathways that match symptom severity with diagnostic priority. For instance, a patient over 45 with rectal bleeding and family history of CRC is directly triaged to colonoscopy.
In complex cases—like anemia with unknown origin, overlapping GI symptoms, or suspected systemic disease—both procedures may be performed during the same visit under combined sedation protocols in advanced UAE GI centers.
Matching symptoms to the right endoscopic tool ensures faster diagnoses, safer care, and reduced need for redundant imaging.
What are the main types of endoscopic procedures?
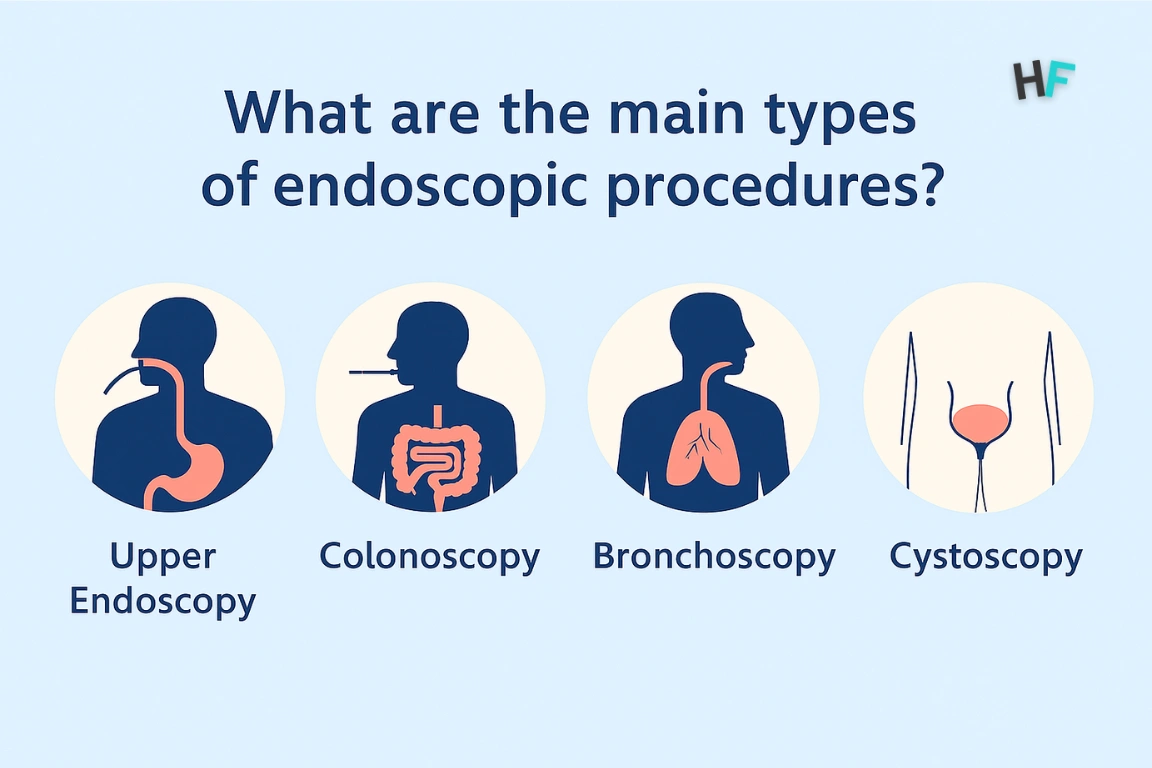
Endoscopic procedures are categorized based on which part of the digestive tract they examine and their clinical purpose. Here are the most common types performed in UAE hospitals:
Gastroscopy (Upper GI Endoscopy)
- Examines: Esophagus, stomach, duodenum
- Used for: Chronic dyspepsia, ulcers, upper GI bleeding
- Local Insight: Widely used in UAE for early gastric cancer screening among high-risk expat groups.
Colonoscopy (Full Colon)
- Examines: Colon and rectum
- Used for: CRC screening, IBD, rectal bleeding
- Dual Role: Diagnostic + polyp removal
- Available in: Public and private hospitals across Dubai, Abu Dhabi, Sharjah, RAK.
Sigmoidoscopy (Partial Colon)
- Examines: Rectum and sigmoid colon only
- Used for: Left-sided abdominal pain, early bleeding
- Benefit: Shorter duration and minimal prep
Capsule Endoscopy
- Examines: Entire GI tract, especially small intestine
- Used for: Obscure GI bleeding, Crohn’s, iron-deficiency anemia
- UAE Use: Offered in advanced referral centers; highly selective.
Endoscopic Ultrasound (EUS)
- Combines: Endoscopy + ultrasound
- Used for: Pancreatic lesions, GI cancer staging
- Centers: Growing in UAE’s tertiary oncology and hepatology clinics.
UAE gastroenterology units now offer these procedures under centralized triage systems, ensuring rapid access to the right diagnostic tool based on symptoms and risk factors.
How are endoscopy and colonoscopy performed?
Both endoscopy and colonoscopy are performed using flexible, camera-equipped instruments inserted into the gastrointestinal tract to directly visualize mucosal surfaces. Though they follow a similar technological principle—real-time endoscopic visualization—the procedural approach, anatomical route, patient positioning, and sedation requirements differ significantly. In the UAE, these procedures are typically performed in hospital-based endoscopy suites under specialist supervision, supported by anesthesiology and pathology teams to ensure safety, comfort, and diagnostic accuracy.
Endoscopy, or upper GI endoscopy (esophagogastroduodenoscopy), is conducted with the patient lying in the left lateral decubitus position. After confirming fasting status and obtaining informed consent, a topical throat anesthetic is applied to reduce the gag reflex, and conscious sedation is administered intravenously. Once relaxed, a thin, flexible endoscope is gently inserted through the mouth and advanced sequentially through the esophagus, stomach, and duodenum. The physician carefully inspects each segment for erosions, ulcers, tumors, or mucosal abnormalities. If suspicious areas are found, biopsies are taken using forceps passed through the endoscope’s working channel. The entire procedure typically lasts 10–20 minutes, after which the patient is monitored for 30–60 minutes before discharge. UAE hospitals often provide a printed or digital report with annotated images on the same day.
Colonoscopy is more complex due to its anatomical path and longer duration. The patient is placed in the left lateral position, and after initiating moderate or deep sedation, the colonoscope is inserted through the anus. The scope is navigated gently through the rectum and colon, with insufflation—preferably CO₂ instead of air—used to expand the bowel lumen for better visibility. Each section of the colon is examined systematically: rectum → sigmoid → descending → transverse → ascending → cecum. Where necessary, the scope may be advanced into the terminal ileum to investigate small bowel pathology. Real-time interventions such as polyp removal (polypectomy), tissue biopsy, tattooing of suspicious lesions, or hemostasis can be performed during the same session. In UAE hospitals, colonoscopies often use AI-assisted polyp detection software, enhancing adenoma detection rates (ADR), especially during screening programs.
Both procedures require sterile conditions and skilled operators, with patient safety protocols embedded throughout. Pre-procedure evaluations include review of medical history, allergies, and current medications, particularly anticoagulants or antiplatelets. Emergency protocols are also in place for rare complications such as perforation or bleeding. Recovery protocols emphasize hydration, light diet, and monitoring for any delayed symptoms such as abdominal pain or persistent bleeding.
In structured GI centers across the UAE—such as Mediclinic, NMC Royal, Burjeel Medical City, and Cleveland Clinic Abu Dhabi—the procedural workflow is standardized to minimize wait times, optimize diagnostic yield, and enhance patient comfort. Bilingual nursing teams, digital scheduling platforms, and cross-specialty integration with hepatology, oncology, or nutrition services ensure that endoscopy and colonoscopy are not isolated procedures, but integrated steps in comprehensive digestive care.
What preparation is required before endoscopy & colonoscopy procedures?
The success of both endoscopy and colonoscopy is highly dependent on proper patient preparation. Inadequate prep can obscure visualization, reduce diagnostic accuracy, and lead to rescheduling, procedural delays, or false-negative findings. Preparation protocols differ for upper and lower GI procedures due to the anatomical path, required visibility, and intervention potential. In UAE healthcare systems, preparation is standardized through pre-procedure checklists, bilingual nursing guidance, and digital reminders, ensuring patient compliance and procedural efficiency.
For endoscopy, preparation is relatively simple but still critical. Patients are required to fast for 6 to 8 hours before the procedure to ensure the stomach is empty. This includes refraining from both food and liquids—especially milk, juices, or coffee, which can interfere with mucosal visibility. Water may be allowed up to 2 hours before the procedure, depending on sedation type and hospital protocol. The reason for fasting is to minimize the risk of aspiration during sedation and to allow the endoscopist a clear view of the stomach and duodenum. Patients on medications such as blood thinners, insulin, or anti-epileptics are advised to consult their doctor for possible dose adjustment or temporary discontinuation. In UAE hospitals, patients receive a pre-procedure call 24 hours in advance, during which medication and fasting instructions are confirmed in their preferred language (Arabic, English, Hindi, or Urdu).
Preparation for colonoscopy is more extensive. The colon must be completely cleared of stool to ensure adequate visualization of mucosal surfaces and to allow for polyp detection, lesion biopsy, or therapeutic intervention. This is achieved through a bowel cleansing regimen that begins one day before the procedure. The most common prep agents in UAE hospitals are polyethylene glycol (PEG)–based solutions, often in split doses—one in the evening before the procedure and the second in the early morning. Patients are instructed to follow a clear liquid diet 24 hours before the procedure, avoiding any red or purple fluids that may mimic blood. Solid food must be avoided entirely.
In certain cases, sodium picosulfate or sodium phosphate-based alternatives may be prescribed, especially for patients with poor tolerance to PEG. However, these are avoided in elderly patients or those with kidney impairment due to the risk of electrolyte imbalance. Patients are also counseled to stay near a restroom once the laxatives are initiated, as multiple bowel movements and cramping are expected. Hydration is emphasized to prevent dehydration during the preparation process.
In both procedures, pre-anesthesia screening includes checking vital signs, reviewing allergies, evaluating sedation fitness, and obtaining signed informed consent. Many UAE facilities use online consent forms, digital appointment tracking, and nurse-led teleconsultations to improve procedural readiness. Some hospitals also provide printed or app-based preparation instructions translated into multiple languages to improve understanding among expatriate populations.
Ultimately, preparation is not just about bowel or stomach clearance—it reflects a structured patient engagement protocol that reduces procedural complications, improves image quality, and allows for complete diagnostic coverage. In UAE’s advanced gastroenterology settings, pre-procedure compliance is treated as a shared responsibility between patient, provider, and care coordinator—aligned with the country’s broader goals of precision medicine and proactive health screening.
What technologies are used in UAE hospitals for endoscopy & colonoscopy?
Modern endoscopy and colonoscopy procedures in the UAE are powered by advanced imaging systems, AI-assisted detection software, and high-performance diagnostic platforms that improve lesion visibility, procedural safety, and diagnostic yield. Hospitals across Dubai, Abu Dhabi, Sharjah, and Ajman have adopted a range of endoscopic technologies that align with international standards while adapting to the UAE’s multiethnic patient base, multilingual workflows, and centralized health records ecosystem.
The most widely used imaging system across UAE hospitals is the Olympus EVIS EXERA III platform, a high-definition endoscopy solution that enables superior mucosal visualization with enhanced contrast. These scopes are equipped with Narrow Band Imaging (NBI), which uses specific light wavelengths to highlight vascular and mucosal structures. NBI significantly improves early detection of precancerous lesions in the esophagus, stomach, and colon—especially in patients undergoing surveillance for Barrett’s esophagus, gastric intestinal metaplasia, or colorectal polyps. Most UAE GI units treat NBI as a first-line enhancement tool during both diagnostic and surveillance procedures.
In colonoscopy, AI-based polyp detection systems—such as CAD EYE (Fujifilm) or ENDO-AID CADe (Olympus)—are being increasingly integrated. These systems use machine learning algorithms trained on global polyp image datasets to provide real-time alerts when abnormal mucosal structures or flat lesions are detected. UAE institutions like Cleveland Clinic Abu Dhabi and Mediclinic Parkview Hospital have begun leveraging these AI overlays to improve adenoma detection rates (ADR), which directly correlates with reduced colorectal cancer risk in population screening cohorts.
Another notable advancement in UAE practice is the shift from air insufflation to carbon dioxide (CO₂) insufflation during colonoscopy. CO₂ is absorbed by the intestinal lining faster than air, which results in less post-procedure discomfort, reduced bloating, and shorter recovery time. Most tertiary endoscopy centers in the UAE now use automatic CO₂ regulators with built-in safety features to maintain patient comfort throughout the procedure.
UAE hospitals also routinely deploy endoscopic biopsy forceps, polypectomy snares, and electrocautery systems through the scope’s working channel, enabling on-the-spot tissue resection, cauterization, and hemostasis. Some endoscopy units are further equipped with dual-channel scopes, which allow two instruments to be used simultaneously—useful during complex procedures like large polyp removal or foreign body retrieval.
On the data and reporting side, UAE healthcare systems have adopted integrated digital endoscopy suites connected to centralized hospital EMR systems such as Cerner, Epic, or TrakCare. This ensures that annotated scope images, biopsy requests, and procedural notes are instantly uploaded and accessible to referring physicians, oncologists, or nutritionists. Patients are often given access to reports through hospital apps or secure email portals, promoting transparency and continuity of care.
In elite GI centers, capsule endoscopy systems (e.g., PillCam SB3) and endoscopic ultrasound (EUS) platforms with high-frequency radial and linear probes are used for advanced diagnostics—particularly in patients with suspected small bowel bleeding or pancreatic lesions. These are typically housed in referral centers or oncology-affiliated units due to their high cost and specialist training requirements.
Together, these technologies form the backbone of a diagnostic ecosystem in the UAE that prioritizes early detection, procedural precision, and system-wide integration. The goal is not just to examine the GI tract—but to do so early, efficiently, and with predictive accuracy, using every digital and optical advantage available.
How do endoscopy & colonoscopy procedures enable early cancer detection?
Endoscopy and colonoscopy are not merely diagnostic tools—they are frontline instruments in preventive oncology, enabling the detection of gastrointestinal cancers at stages where intervention is curative rather than palliative. Their clinical value lies in the ability to visualize precancerous lesions, retrieve tissue for histopathology, and, in many cases, remove the lesion entirely before malignant transformation occurs. In the UAE, where the incidence of gastric and colorectal cancers is steadily rising due to changing lifestyles, dietary patterns, and genetic predisposition in multiethnic populations, these procedures are embedded into the national cancer screening agenda.
Upper GI endoscopy plays a pivotal role in detecting esophageal and gastric cancers, particularly in patients presenting with chronic dyspepsia, persistent vomiting, unexplained weight loss, or gastrointestinal bleeding. Conditions such as Barrett’s esophagus—a known precursor to esophageal adenocarcinoma—can be monitored through periodic gastroscopy with targeted biopsies. Similarly, intestinal metaplasia and dysplastic gastric polyps, when identified early via endoscopy, allow physicians to initiate surveillance or curative endoscopic mucosal resection (EMR), reducing progression to invasive gastric cancer. In high-risk demographics, especially East Asian expatriates in the UAE, routine endoscopy is increasingly recommended for those over 40 with persistent upper GI symptoms.
Colonoscopy is the gold standard for colorectal cancer (CRC) detection and prevention. It is the only diagnostic tool that allows visual identification, risk stratification, biopsy, and removal of polyps in a single procedure. The majority of CRC cases arise from adenomatous polyps, which progress to malignancy over a 5–10 year window. Detecting and excising these polyps through colonoscopy effectively interrupts this transformation sequence. In the UAE, CRC screening is recommended starting at age 45, and earlier for those with family history or hereditary syndromes like Lynch syndrome or FAP (familial adenomatous polyposis).
Colonoscopy also detects flat lesions, serrated adenomas, and right-sided cancers, which are often missed by fecal occult blood tests or imaging. With the addition of AI-driven polyp detection systems, UAE hospitals now achieve higher adenoma detection rates (ADR), directly correlating with reduced cancer incidence in population-level studies. Moreover, tissue samples obtained during colonoscopy are analyzed by UAE-based histopathology labs within 48–72 hours, allowing oncologists and surgeons to make rapid treatment decisions if malignancy is confirmed.
Both procedures also support cancer staging and post-treatment surveillance. Endoscopy is used to evaluate tumor margins, gastric outlet obstruction, or post-gastrectomy anatomy, while colonoscopy assesses post-surgical anastomosis, metachronous polyps, or recurrence. These scopes can also be enhanced with chromoendoscopy or narrow-band imaging (NBI) for better detection of early mucosal changes.
The integration of endoscopy and colonoscopy into UAE’s digital health systems ensures that screening, diagnostic reporting, and follow-up surveillance are traceable and coordinated. At-risk patients flagged in centralized EMR systems can be scheduled for repeat scopes at evidence-based intervals, making cancer prevention a proactive, protocol-driven process rather than a reactive one.
Ultimately, the ability of these procedures to detect cancer in its earliest stages—when confined to the mucosa, before nodal spread or systemic involvement—translates to higher cure rates, less invasive treatment, and better survival outcomes. In the UAE’s population health strategy, they are not optional investigations; they are strategic interventions aimed at reducing disease burden and improving national cancer statistics.
What happens after the endoscopy and colonoscopy procedure?
The post-procedure phase of both endoscopy and colonoscopy begins with clinical monitoring, followed by sedation recovery, diagnostic reporting, and patient instruction. While the procedures themselves are brief and minimally invasive, the aftercare phase is critical for identifying complications early, ensuring patient safety, and enabling timely follow-up. In the UAE’s structured healthcare system, recovery is supervised by bilingual nursing teams trained in sedation protocols, discharge planning, and patient education.
After upper GI endoscopy, patients are transferred to a post-anesthesia care unit (PACU) where they are monitored for 30–60 minutes. Vital signs, oxygen saturation, and neurological responsiveness are continuously assessed. Throat numbness from local anesthetic may persist temporarily, and mild bloating or burping is common due to air insufflation during the procedure. Patients are usually advised to avoid eating or drinking for at least one hour until the gag reflex fully returns. In most UAE hospitals, same-day discharge is standard unless complications such as significant bleeding or severe findings warrant observation or hospital admission.
For colonoscopy, the recovery window is slightly longer—ranging from 60 to 90 minutes—especially when deep sedation or polypectomy has been performed. Patients may experience temporary abdominal cramps, flatulence, or fatigue, all of which resolve spontaneously. Those who underwent biopsy or polyp removal are instructed to avoid blood-thinning medications, heavy lifting, or strenuous activity for 24–48 hours. UAE protocols require a responsible adult to accompany the patient home due to lingering sedation effects, and most facilities prohibit driving for the rest of the day.
Both procedures include a verbal debrief from the performing gastroenterologist immediately after recovery, often accompanied by annotated still images taken during the scope. However, biopsy results—if taken—are not available immediately. UAE labs typically process and release histopathology findings within 2 to 5 working days, depending on urgency and insurance authorization for special stains or immunohistochemistry.
Patients are given a discharge report, which includes:
- Procedure summary
- Findings and provisional diagnosis
- Biopsy sites (if applicable)
- Medication changes (e.g., PPIs, antibiotics, iron supplementation)
- Follow-up instructions and scope surveillance interval
In leading UAE hospitals, this report is shared digitally via patient portals, mobile health apps, or secure email, enabling access by referring physicians, dietitians, or oncologists involved in the care pathway. For example, if intestinal metaplasia is detected on endoscopy, the patient is booked for surveillance endoscopy every 2–3 years based on international guidelines. Similarly, adenomatous polyps found during colonoscopy will trigger risk-based recall cycles—typically 3, 5, or 10 years—depending on size, number, and dysplasia grade.
Complication monitoring is part of standard post-discharge protocol. Patients are instructed to report symptoms such as persistent abdominal pain, rectal bleeding, vomiting, chest discomfort, or fever, which may indicate rare but serious complications such as perforation, hemorrhage, or post-polypectomy syndrome. Most UAE facilities have 24/7 helplines, emergency backup coverage, and teleconsultation options to support post-endoscopy triage if symptoms arise.
Recovery after endoscopy or colonoscopy is usually quick, with most patients resuming normal activity within a day. However, for procedures requiring follow-up, like polypectomy or GI bleed control, rehabilitation guidance becomes essential — just as in orthopedic recovery pathways. You may also explore structured post-op stages in the ACL Tear Recovery Timeline that maps surgery-to-physiotherapy phases.
In the UAE’s quality-regulated healthcare model, the procedure doesn’t end in the endoscopy room—it continues through structured post-procedure tracking, pathology correlation, and guideline-driven surveillance scheduling. This continuity reinforces the diagnostic value of scopes and builds patient trust, especially in a multicultural patient population unfamiliar with preventive interventions.
Are endoscopy and colonoscopy safe?
Endoscopy and colonoscopy are considered highly safe and routinely performed procedures across global healthcare systems, including the UAE. When conducted by trained gastroenterologists in accredited endoscopy units, the risk of serious complications is exceptionally low. These procedures are governed by standard operating protocols, anesthesia guidelines, and adverse event mitigation systems, all of which are strictly enforced in UAE’s licensed healthcare facilities.
The most common side effects are mild and transient, including bloating, throat irritation (in endoscopy), or temporary abdominal discomfort (in colonoscopy). These are expected physiological responses to the insufflation of air or carbon dioxide during the procedure. In the vast majority of cases, these symptoms resolve within a few hours and require no treatment.
Serious complications are rare, but not nonexistent. In upper GI endoscopy, the risk of perforation is estimated at less than 1 in 10,000 cases, and the risk of significant bleeding (typically post-biopsy or in variceal banding) is similarly low. In colonoscopy, the perforation risk ranges between 1 in 1,000 to 1 in 3,000, depending on whether a polypectomy or therapeutic intervention was performed. Bleeding after polyp removal occurs in 0.2% to 2% of cases and is usually self-limiting or managed endoscopically.
In the UAE, these risk parameters are closely monitored by hospital accreditation bodies such as the Department of Health – Abu Dhabi (DOH) and Dubai Healthcare City Authority (DHCA). Licensed gastroenterology centers are required to report adverse events, maintain complication logs, and follow audit trails for every endoscopic intervention. These systems ensure accountability, improve training, and enable early identification of process breakdowns.
To further enhance procedural safety, UAE hospitals adhere to sedation safety guidelines based on American Society of Anesthesiologists (ASA) scoring. Patients with known cardiovascular, pulmonary, or bleeding disorders undergo pre-procedure clearance. Anticoagulation protocols are strictly followed, and medications like warfarin or DOACs are paused or bridged only under physician supervision. For high-risk patients, scopes may be performed in operating room settings with anesthesiology backup, especially in tertiary care centers such as Cleveland Clinic Abu Dhabi or Mediclinic City Hospital.
Technology also plays a role in reducing risk. The use of CO₂ insufflation, which is rapidly absorbed by the bowel lining, minimizes the risk of post-procedure pain and perforation compared to traditional air-based insufflation. Disposable biopsy forceps, sterile accessories, and validated reprocessing workflows ensure that infection risk is negligible. Cross-contamination events are virtually eliminated in UAE hospitals due to rigid endoscope sterilization protocols that meet international Joint Commission International (JCI) standards.
Importantly, the overall risk-benefit ratio of both procedures heavily favors intervention, particularly when evaluating for malignancy, bleeding, or chronic inflammation. Delaying or avoiding endoscopy or colonoscopy due to fear of complications often results in diagnostic delay, more advanced disease stages, and increased healthcare burden.
In summary, while no procedure is risk-free, endoscopy and colonoscopy, when performed within UAE’s regulated healthcare framework, are exceptionally safe, meticulously controlled, and predictably effective. The focus is not just on risk avoidance—but on risk governance, which integrates patient history, procedural indication, operator skill, and technological safeguards into a seamless care experience.
What are the cost and insurance coverage in the UAE?
The cost of endoscopy and colonoscopy in the UAE varies based on procedure type, hospital tier, insurance provider, sedation method, and whether a biopsy or therapeutic intervention is performed. While both procedures are widely available across public and private sectors, pricing differs significantly between self-pay and insurance-covered patients, and between standard diagnostics and advanced imaging-enhanced scopes.
For self-paying patients, the average cost of upper GI endoscopy ranges from AED 1,000 to AED 3,000. This typically includes consultation, procedure fees, standard sedation, and image documentation. In contrast, colonoscopy costs range between AED 1,800 and AED 5,000, with variability driven by the use of CO₂ insufflation, polypectomy kits, or histopathology charges. Capsule endoscopy and endoscopic ultrasound (EUS), used in specialized centers, are priced higher—often exceeding AED 7,000—due to imported equipment, single-use accessories, and extended interpretation time.
For insured patients, the coverage pathway depends on medical necessity, policy type (basic vs comprehensive), and whether the procedure is classified under diagnostic or preventive benefits. Most UAE insurance providers—including Daman, Thiqa, AXA Gulf, Oman Insurance, MetLife, and Bupa—cover both procedures when there is a valid referral and ICD-10 justification code (e.g., R19.7 for diarrhea, K21.9 for reflux, or Z12.11 for CRC screening). In such cases, pre-approval is often required, and the claim must be submitted via eClaimLink or Shafafiya portals for digital adjudication.
Preventive screening colonoscopy, especially for individuals aged 45 and above, is increasingly reimbursed under wellness and early detection programs—particularly under Thiqa plans for Emirati nationals or employer-based platinum policies. If the procedure is performed as part of an annual health check-up, it may be billed under bundled preventive services, especially in hospitals aligned with corporate wellness partnerships.
However, scope procedures without strong symptomatic justification—such as anxiety-driven requests for routine endoscopy or asymptomatic young patients seeking early CRC screening—may not be covered, or may require co-payments of 10–20%, depending on insurer rules. Most hospitals in the UAE offer insurance coordination desks and prior authorization officers to assist patients in understanding cost implications before confirming scope bookings.
For patients without insurance or with international policies not aligned to UAE networks, hospitals like NMC Royal, Medeor, Aster, or Ahalia offer cash packages that include doctor consultation, scope procedure, sedation, and reporting. These are typically discounted and pre-paid, ranging from AED 1,500 to AED 3,500 for endoscopy, and AED 2,500 to AED 5,500 for colonoscopy, depending on the inclusion of biopsy and histopathology charges.
It is important to note that biopsies, polyp histology, and repeat follow-ups are often billed separately unless bundled. Additionally, if complications occur (e.g., bleeding requiring clipping or extended recovery), supplementary charges may apply, which are either billed under insurance extensions or disclosed to cash-paying patients before intervention.
Patients often compare diagnostic and surgical costs when making decisions about gastrointestinal or orthopedic procedures. Similar to how insurance covers endoscopy or colonoscopy in specific clinical scenarios, those undergoing major orthopedic procedures can refer to our detailed breakdown of the Knee Replacement Surgery Cost in UAE — including packages, types, and post-operative support.
In summary, UAE’s cost structure for endoscopy and colonoscopy reflects a hybrid model—where early detection is prioritized by major insurers, but procedural efficiency, documentation, and code justification determine reimbursement eligibility. Patients are advised to consult both their insurer and hospital billing coordinator prior to scheduling, ensuring that pricing, coverage, and out-of-pocket exposure are fully transparent.
Can both procedures be done on the same day?
Yes, both endoscopy and colonoscopy can be performed on the same day, provided the clinical indication justifies dual examination and the patient is appropriately prepped for both upper and lower GI tract evaluation. In UAE hospitals, same-day combined procedures are increasingly common, especially in patients presenting with non-specific gastrointestinal symptoms, obscure GI bleeding, iron-deficiency anemia, or when completing a full GI workup before surgery, transplant evaluation, or systemic disease screening.
The decision to schedule both scopes in a single session is based on multiple predicates:
- Symptom overlap (e.g., bloating, weight loss, anemia without known source)
- Time efficiency for international patients or those on short visits
- Insurance pathway optimization (one-day authorization, bundled sedation)
- Patient convenience, especially for elderly or chronically ill individuals
From a procedural standpoint, upper GI endoscopy is performed first, followed immediately by colonoscopy while the patient remains sedated. This sequence prevents contamination of the upper airway from residual laxatives and reduces anesthesia turnaround time. Both scopes are done under conscious or deep sedation, typically midazolam–fentanyl or propofol-based protocols, depending on patient ASA status and hospital sedation policy.
In the UAE, hospitals such as Mediclinic City Hospital, American Hospital Dubai, Burjeel Medical City, and Cleveland Clinic Abu Dhabi offer combined scope scheduling with pre-bundled anesthesia, post-procedure monitoring, and unified digital reporting. This model allows for single-day discharge, consolidated recovery, and a full endoscopy suite report with annotated images, preliminary findings, and biopsy notes delivered the same day via hospital apps or printed summaries.
However, successful same-day procedures require dual preparation protocols. Patients must follow standard bowel cleansing with PEG solution (for colonoscopy) while also fasting from solids and liquids (for endoscopy). This preparation is usually supervised by endoscopy coordinators or nursing navigators, who ensure compliance with dietary restrictions and medication adjustments, including temporary discontinuation of anticoagulants, NSAIDs, or diabetic medications if needed.
Not all patients are suitable for same-day combined procedures. Contraindications include poor sedation tolerance, hemodynamic instability, recent myocardial infarction, or known airway anomalies. For these individuals, staging the procedures on different days under focused pre-anesthetic assessment is preferred. Additionally, in low-resource settings or smaller outpatient units without anesthesiology backup, combined scopes may not be feasible due to workflow constraints.
From a cost-efficiency perspective, combining scopes into a single session can reduce overall expenditure for insured and self-paying patients. While the total procedural charge may be slightly higher than for a single scope, bundled billing typically reduces duplication of anesthesia fees, recovery costs, and nursing hours. Some UAE insurance plans even prefer this approach to limit repeated authorization cycles and day-care admissions.
Ultimately, same-day endoscopy and colonoscopy reflect the UAE’s push toward integrated diagnostics, particularly in multidisciplinary units managing liver disease, anemia workups, IBD clinics, or pre-bariatric surgery assessments. When clinically appropriate, it compresses the diagnostic timeline, reduces patient anxiety, and accelerates therapeutic decision-making—especially in cases where delayed diagnosis could lead to preventable complications.
How do gastroenterologists decide between endoscopy and colonoscopy?
Gastroenterologists decide between endoscopy and colonoscopy by mapping the patient’s symptom profile, risk category, and anatomical location of concern to the most appropriate diagnostic route. The decision is not arbitrary—it is an outcome of a structured clinical algorithm that stratifies presenting complaints into upper versus lower gastrointestinal origin, overlaid with red-flag indicators, medication history, age, and family risk. In the UAE’s tertiary care model, this triage system is often embedded into internal medicine referral templates, ensuring precision in both investigation and insurance pre-approval.
Upper GI symptoms—those localizing to the esophagus, stomach, or duodenum—trigger a referral for gastroscopy (upper endoscopy). These include:
- Persistent heartburn not responding to proton pump inhibitors (PPIs)
- Upper abdominal pain, especially post-meal epigastric discomfort
- Difficulty swallowing (dysphagia) or painful swallowing (odynophagia)
- Nausea and vomiting of unknown cause
- Suspected upper GI bleeding (e.g., black stools, coffee-ground emesis)
- Surveillance in Barrett’s esophagus or gastric intestinal metaplasia
In contrast, symptoms pointing to colonic or rectal origin drive the need for colonoscopy. These include:
- Rectal bleeding (fresh blood or blood mixed with stool)
- Changes in bowel habits (e.g., persistent diarrhea, new-onset constipation)
- Lower abdominal cramping, bloating, or incomplete evacuation
- Positive fecal occult blood test (FOBT) or fecal immunochemical test (FIT)
- Iron-deficiency anemia with no apparent upper GI source
- Family history of colorectal cancer or polyps
- Surveillance for known Inflammatory Bowel Disease (IBD)
When symptoms overlap—such as in patients with chronic anemia or vague abdominal discomfort—gastroenterologists may opt to perform both scopes either sequentially or in the same session. This dual diagnostic strategy is especially common in undiagnosed gastrointestinal bleeding, suspected celiac disease with anemia, or in pre-transplant evaluations where a complete GI workup is protocolized.
Clinical context modifies the decision further. A 50-year-old patient with left-sided abdominal pain and altered bowel habits will likely be triaged to colonoscopy to exclude colonic malignancy or diverticulosis. A 40-year-old with epigastric pain, nausea, and long-term NSAID use would be better served with endoscopy to evaluate for peptic ulcer disease. In pediatric cases, scopes are used selectively and almost always based on pediatric GI specialist consultation due to sedation risk and anatomical considerations.
In the UAE, this decision-making process is augmented by centralized referral triage, especially in insurance-based care. Physicians are required to specify ICD-10 codes, symptom duration, prior interventions, and lab/imaging findings to justify the choice of scope. This level of documentation ensures insurance approval and supports the hospital’s utilization review process. Some hospitals even use symptom-to-scope decision matrices built into EMR systems, prompting the referrer to justify the choice via checklists or pre-filled templates.
Ultimately, choosing between endoscopy and colonoscopy is not a matter of availability—it is an evidence-driven alignment between symptoms, anatomical suspicion, diagnostic yield, and clinical urgency. In structured GI programs across the UAE, this decision tree is automated, auditable, and optimized to reduce time-to-diagnosis and minimize procedural redundancy.
Who should undergo routine colonoscopy screening in the UAE?
Routine colonoscopy screening in the UAE is recommended for adults who fall into defined risk categories for colorectal cancer (CRC)—a leading cause of cancer-related deaths both globally and within the Emirates. The decision to initiate screening is based not solely on age, but also on family history, ethnicity, symptom profile, and predisposing conditions such as inflammatory bowel disease (IBD) or hereditary cancer syndromes. In the UAE’s public and private healthcare systems, colonoscopy is increasingly integrated into preventive health checkups, insurance-based wellness programs, and national cancer control strategies led by entities like the Department of Health – Abu Dhabi (DOH) and the Dubai Health Authority (DHA).
The general population threshold for first-time screening colonoscopy is 45 years of age, aligning with updated global guidelines, including those from the American Cancer Society (ACS). This age applies to asymptomatic, average-risk individuals—those with no personal or family history of colorectal neoplasia, no symptoms, and no inflammatory or genetic predispositions. In these individuals, colonoscopy is recommended once every 10 years if the findings are normal.
Individuals with a first-degree relative diagnosed with colorectal cancer or advanced adenomas (especially before age 60) are classified as moderate to high risk. These patients are advised to begin screening at age 40, or 10 years earlier than the age of diagnosis in the affected relative—whichever comes first. In UAE hospitals, this risk-based rule is encoded in EMR systems to prompt early referral and avoid screening delays.
Patients with chronic inflammatory bowel diseases, such as ulcerative colitis or Crohn’s colitis, are also included in the surveillance cohort. For these individuals, screening begins 8–10 years after disease onset, with repeat colonoscopy every 1–3 years depending on histological findings, presence of pseudopolyps, or biopsy-confirmed dysplasia. UAE-based GI units managing IBD patients typically maintain a surveillance log to trigger follow-up colonoscopies at evidence-based intervals.
Those diagnosed with hereditary syndromes—such as Lynch syndrome (HNPCC) or familial adenomatous polyposis (FAP)—require far more aggressive surveillance. Lynch syndrome carriers begin colonoscopy every 1–2 years from age 20–25, while FAP patients may undergo annual scopes from adolescence, or proceed to prophylactic colectomy if polyp burden is unmanageable. In the UAE, such high-risk cases are referred to tertiary GI genetics centers for integrated surveillance and counseling.
Additionally, any adult—regardless of age—who presents with:
- Unexplained iron-deficiency anemia
- Positive fecal occult blood test (FOBT/FIT)
- Chronic changes in bowel habits
- Rectal bleeding or persistent abdominal pain should undergo diagnostic colonoscopy immediately, even if they do not meet screening age thresholds.
In the UAE’s healthcare context, many insurance policies now cover screening colonoscopy under preventive services—especially Thiqa, Daman Enhanced, and Bupa Global plans. Several hospitals offer direct-access screening programs, where eligible patients can schedule colonoscopy without a prior specialist consult, provided they meet predefined low-risk criteria and pass a sedation fitness screening.
Ultimately, colonoscopy is not a one-size-fits-all tool. Screening must be personalized based on age, risk, and symptom alignment. In the UAE, where CRC incidence is rising and younger demographics are increasingly affected, risk-adjusted colonoscopy access is central to early detection. The goal is not merely to identify cancer—but to intercept the polyp-to-carcinoma sequence long before malignant transformation occurs.
What are alternatives to traditional endoscopy and colonoscopy?
While traditional endoscopy and colonoscopy remain the gold standard for visualizing the gastrointestinal tract, several alternative diagnostic modalities have emerged—offering non-invasive, patient-friendly options with variable sensitivity, specificity, and accessibility. These alternatives are particularly relevant for patients who are sedation-intolerant, high-risk surgical candidates, or non-compliant with bowel prep protocols. In the UAE, where healthcare technology adoption is rapid and patient preferences are diverse, these alternatives are increasingly offered in tertiary centers, albeit with selective use based on clinical indication and diagnostic priority.
Capsule endoscopy is one of the most prominent alternatives for evaluating the small intestine, a region not fully accessible by traditional upper endoscopy or colonoscopy. The procedure involves swallowing a pill-sized wireless camera, which captures high-resolution images as it traverses the GI tract, transmitting data to an external receiver worn by the patient. It is primarily used in patients with obscure gastrointestinal bleeding, suspected small bowel Crohn’s disease, or undiagnosed iron-deficiency anemia. However, it is not suitable for upper GI cancers or colonic polyps, and does not allow biopsy or therapeutic intervention. In the UAE, capsule endoscopy is available at hospitals like Cleveland Clinic Abu Dhabi, Mediclinic City Hospital, and select private gastroenterology clinics.
CT colonography, also known as virtual colonoscopy, is a radiological alternative for imaging the colon using low-dose computed tomography after bowel preparation and gas insufflation. It offers a non-invasive method to detect large polyps and masses without sedation or scope insertion. The test is often used in patients who are unfit for colonoscopy or refuse invasive procedures. However, its diagnostic yield is lower for flat lesions, and any abnormal findings still require a follow-up colonoscopy for biopsy or polyp removal. In UAE radiology units, virtual colonoscopy is available but used sparingly due to its two-step diagnostic nature and limitations in real-time intervention.
Transnasal endoscopy (TNE) is a minimally invasive variation of standard upper endoscopy, performed using an ultra-thin scope inserted through the nose instead of the mouth. It is done without sedation in an outpatient setting and is well tolerated by patients with high gag reflex or sedation contraindications. The drawback lies in reduced image resolution and a narrower working channel, limiting its utility in therapeutic interventions. TNE is not yet widely available in the UAE, though academic institutions and ENT-GI collaboration units are beginning to explore its integration.
Magnetic resonance enterography (MRE) and CT enterography are non-endoscopic imaging techniques used to assess small bowel pathology—particularly in Crohn’s disease. These modalities provide cross-sectional imaging of bowel wall thickness, lymph nodes, and mesenteric vascularity but lack mucosal detail and direct visualization. They are used adjunctively rather than as standalone replacements and are especially useful in IBD surveillance. UAE hospitals with advanced radiology services routinely include MRE in IBD management protocols alongside capsule or colonoscopic evaluation.
Stool-based tests, such as fecal immunochemical test (FIT) or multi-target stool DNA tests (e.g., Cologuard), are increasingly adopted in mass CRC screening programs globally. These tests detect blood or DNA markers shed by colorectal neoplasms. However, their positive predictive value is limited, and a positive result always necessitates colonoscopy for confirmation. While FIT is available in some UAE wellness packages, it has not replaced colonoscopy in any insurance-authorized screening algorithms.
In summary, alternatives to traditional scopes are useful for selected indications, specific anatomical regions, or patient populations with procedural constraints. Yet, their lack of biopsy access, therapeutic limitations, or two-step workflows restrict them from replacing endoscopy or colonoscopy as first-line diagnostic tools. In the UAE’s clinical hierarchy, they function as adjuncts, not substitutes—valuable in selected contexts, but ultimately complementary to full-scope endoscopic evaluation.
What questions should patients ask before undergoing the procedure?
Before undergoing an endoscopy or colonoscopy, patients are encouraged to ask structured, outcome-focused questions that clarify procedural expectations, diagnostic goals, safety measures, and post-procedure responsibilities. This dialogue is not just about informed consent—it’s a critical layer of decision validation in the patient care journey, particularly within the UAE’s multilingual, multi-insurance healthcare ecosystem. Asking the right questions ensures alignment between patient concerns and procedural intent, reduces anxiety, and prevents misunderstandings about cost, sedation, or findings.
What are the specific clinical reasons I need this procedure?
This confirms whether the scope is for diagnosis, cancer screening, surveillance, or preoperative staging. Understanding whether the indication is symptom-driven (e.g., bleeding, reflux, altered bowel habits) or preventive (e.g., family history, anemia) helps patients mentally prepare for potential findings or follow-up interventions.
What will you be looking for during the procedure?
This clarifies anatomical focus and diagnostic targets—such as ulcers, polyps, tumors, varices, or inflammatory changes. Patients should know which part of the GI tract will be examined and whether biopsies are expected.
What type of sedation will be used, and what are the risks?
In the UAE, most scopes are performed under conscious or deep sedation, depending on the patient’s medical history and hospital protocols. Patients with heart conditions, respiratory issues, or past sedation reactions should flag this early to ensure pre-anesthetic evaluation.
Do I need to stop any medications before the procedure?
This is essential for patients taking anticoagulants, antiplatelets, insulin, NSAIDs, or iron supplements. Adjustments may be required to minimize bleeding risk or avoid adverse drug interactions during sedation. Most UAE hospitals provide a medication reconciliation call before the procedure.
Will biopsies be taken, and how long will results take?
If a lesion, polyp, or inflamed area is found, biopsy is standard. Patients should ask when and how results will be communicated. In the UAE, most hospitals deliver biopsy results within 2 to 5 working days via patient portals or follow-up appointments.
What should I expect after the procedure in terms of recovery, diet, and follow-up?
Post-procedural symptoms such as bloating, sore throat, or mild cramps are common. Patients should understand discharge timing, when to resume normal diet, and warning signs (e.g., persistent pain, bleeding) that require medical attention.
Will insurance cover the procedure and associated costs?
Patients must ask whether the procedure is pre-approved, what is included (sedation, histopathology), and what is excluded (repeat visits, complications, follow-up imaging). UAE hospitals typically offer billing coordinators to walk patients through policy coverage, exclusions, and co-pay amounts.
If something abnormal is found, what’s the next step?
This sets patient expectations regarding possible escalation—such as surveillance scopes, referral to oncology, diet changes, or medication. It helps avoid information overload post-procedure and provides clarity around contingency plans.
Can this procedure be combined with another to avoid two sessions?
For patients needing both upper and lower GI evaluations, this question allows doctors to determine if a same-day combined procedure is feasible, reducing cost and sedation exposure.
How experienced is the endoscopist, and how often is this procedure performed here?
While all licensed UAE hospitals meet safety standards, asking about procedural volume and expertise helps patients feel more confident. High-volume centers often have better safety outcomes, faster reporting, and dedicated support staff.
In UAE’s multilingual, technology-driven care environment, asking these questions ensures procedural clarity, patient safety, and insurance transparency—reinforcing a diagnostic encounter that is informed, efficient, and trust-building.
How has endoscopy evolved historically and in the UAE?
Endoscopy has evolved from a rudimentary inspection method into a high-definition, AI-supported diagnostic and therapeutic platform. This evolution has unfolded over more than a century, driven by advances in optics, miniaturization, image processing, and medical robotics. In the UAE, the adoption of endoscopic technology has accelerated rapidly over the past two decades, with integration into national screening programs, private-sector investment, and regulatory emphasis on early cancer detection. The result is a diagnostic environment where endoscopy is not just a test—it is a structured clinical service aligned with international standards and local population needs.
Historically, the first documented attempts at endoscopy date back to the early 1800s, when rigid metal tubes with mirrors were used to inspect the throat and bladder. These early instruments lacked illumination and were associated with high discomfort and limited diagnostic yield. The introduction of electric light sources in the late 19th century improved visibility but still required patient restraint and surgical exposure.
A turning point came in the 1950s, with the development of flexible fiberoptic endoscopes by Harold Hopkins and Basil Hirschowitz. These scopes allowed real-time visualization of the GI tract without open surgery, transforming gastroenterology into a procedure-oriented specialty. In the 1980s, the shift to video endoscopy—using CCD cameras and external monitors—enabled image documentation, teaching, and multicenter collaboration, laying the groundwork for standardized diagnostics.
By the early 2000s, endoscopy entered the digital era. High-definition video systems, narrow-band imaging (NBI), chromoendoscopy, and therapeutic channels expanded the scope’s role from diagnosis to biopsy, polypectomy, cauterization, and stent placement. Simultaneously, capsule endoscopy and endoscopic ultrasound (EUS) extended visualization beyond the reach of traditional scopes.
In the UAE, endoscopy began as a hospital-based referral procedure but has since evolved into a widely accessible diagnostic service across public and private sectors. Hospitals like Cleveland Clinic Abu Dhabi, Mediclinic Middle East, and Burjeel Medical City now offer advanced endoscopy suites equipped with:
- Olympus EVIS EXERA III/NBI platforms
- AI-assisted polyp detection systems
- Dual-channel therapeutic endoscopes
- CO₂ insufflation for comfort
- Fully integrated EMR-linked reporting
The Dubai Health Authority (DHA) and Department of Health – Abu Dhabi (DOH) have embedded endoscopy and colonoscopy into their national screening guidelines, especially for colorectal cancer and chronic liver disease evaluation. Routine colonoscopy is now offered as part of Thiqa and Daman wellness programs, and endoscopy is the frontline tool for investigating persistent upper GI symptoms, particularly in high-risk ethnic groups.
Telemedicine has further extended endoscopy’s reach. In UAE tertiary centers, digital scope reports with annotated images are automatically uploaded to EMRs and shared with referring physicians or specialists for coordinated follow-up. This data integration ensures that biopsies, pathology results, surveillance planning, and patient education are linked to a single diagnostic event.
Looking forward, UAE hospitals are preparing for the next generation of endoscopy, including:
- AI-enhanced lesion classification (beyond detection)
- 3D mapping of the mucosal surface
- Robotic endoscopy for remote navigation
- Real-time histological prediction via endomicroscopy
Thus, endoscopy in the UAE has transitioned from a procedural service to a multi-modal diagnostic platform, supported by technology, protocols, and policy. Its evolution reflects the UAE’s broader healthcare vision: fast, precise, digital-first, and patient-centered.
What is the future of endoscopic procedures in the UAE?
The future of endoscopic procedures in the UAE is being shaped by the convergence of cutting-edge technologies, precision diagnostics, and integrated healthcare ecosystems. Both public and private sectors are increasingly focused on deploying innovations that enhance early detection, improve patient experience, and support long-term prognostic monitoring—all aligned with the UAE’s strategic move toward a digital-first, preventive medicine landscape.
AI-powered lesion detection and classification will likely become routine in the near future. Advanced artificial intelligence systems are being trained to not only detect polyps during colonoscopy, but also differentiate between benign and malignant tissue in real time. Trials are ongoing in major centers—such as Cleveland Clinic Abu Dhabi and Mediclinic—to validate AI algorithms that can accurately characterize adenomas vs serrated lesions and determine optimal biopsy sites before histology is available.
Robotic and capsule-assisted endoscopy represent another frontier. Miniaturized robotic capsules equipped with micro-motors and real-time imaging are under investigation for controlled navigation through the GI tract. While still requiring clinical validation, these devices promise to improve access in difficult-to-reach regions and may reduce the need for sedation. UAE-based research institutions are partnering with international manufacturers to pilot these devices within the next 3–5 years.
3D mucosal mapping and endomicroscopy are enhancing diagnostic precision by providing optical biopsy capabilities—essentially allowing microscopic evaluation of tissue during the procedure. This can reduce unnecessary tissue removal and improve targeted surveillance, particularly for dysplasia in Barrett’s esophagus or inflammatory bowel disease. High-end tertiary hospitals in the UAE are exploring confocal laser endomicroscopy systems integrated into their endoscopy suites.
Integration with hospital EMR systems will grow more intelligent. Future scope reports will include not only annotated images, but also structured data for predictive analytics. For example, patient risk profiles—including age, family history, polyp type, and histology—will feed into automatic recall scheduling systems, reducing oversights and ensuring compliance with international follow-up guidelines.
Tele-endoscopy, where live procedures are streamed to remote experts for guidance or second opinions, represents another powerful tool for expanding capability across the UAE. Rural hospitals or satellite centers will benefit from real-time support from specialist gastroenterologists in larger facilities, improving diagnostic accuracy and procedural safety in lower-resource settings.
Finally, the future is shaped by AI-assisted training and credentialing. Virtual reality (VR)-based simulation and machine-learning evaluation of procedural skill will play a key role in credentialing UAE endoscopists. Centers like Burjeel and Aster are already piloting simulation-based training programs, ensuring consistency and patient safety across the region.
What are the pros and cons of endoscopy vs colonoscopy?
Endoscopy and colonoscopy each offer unique diagnostic strengths aligned with different anatomical zones of the gastrointestinal tract. The choice between them is determined by symptom location, patient history, and the clinical goal—whether diagnostic, surveillance, or therapeutic. While both procedures use similar technologies, their patient preparation requirements, procedural scope, risks, and intervention capacities differ. In UAE healthcare settings, the ability to select the right modality based on benefit–burden ratio is critical for maximizing diagnostic yield while minimizing discomfort and procedural risk.
Below is a structured overview of the advantages and limitations of each procedure:
| Aspect | Endoscopy (Upper GI) | Colonoscopy (Lower GI) |
|---|---|---|
| Primary Diagnostic Area | Esophagus, stomach, duodenum | Colon, rectum, terminal ileum |
| Procedure Duration | Shorter (15–20 minutes) | Longer (30–60 minutes) |
| Preparation Needed | Fasting (6–8 hours) | Full bowel prep (PEG solution) |
| Sedation Requirement | Conscious sedation (mild) | Moderate to deep sedation |
| Cancer Screening Role | Gastric/esophageal (symptom-based) | Colorectal (routine from age 45) |
| Therapeutic Capabilities | Ulcer biopsy, banding, dilation | Polyp removal, biopsy, tattooing |
| Post-Procedure Comfort | Minimal (sore throat, bloating) | Mild cramps, gas for 24–48 hrs |
| Technology Enhancements | NBI, AI lesion detection | AI colonoscopes, CO₂ inflation |
| Complication Risk | <0.1% (rare bleeding/perforation) | 0.1–0.3% (higher with polypectomy) |
| Insurance in UAE | Covered if justified (GERD, ulcers) | Often encouraged and covered |
| Patient Recall Cycle | Only if disease found | 3–10 years based on findings |
| Limitations | Does not view lower GI tract | Cannot evaluate esophagus/stomach |
Which hospitals in the UAE are best known for GI endoscopy?
The UAE is home to several internationally accredited hospitals and specialty centers that have established strong reputations in gastrointestinal endoscopy. These institutions are distinguished not only by the volume and complexity of procedures performed, but also by their integration of advanced imaging technologies, AI-assisted diagnostics, and structured follow-up systems. Referrals from both general practitioners and internal medicine specialists converge toward these centers due to their procedural safety, multi-specialist teams, and streamlined insurance coordination.
Cleveland Clinic Abu Dhabi is widely recognized as one of the region’s premier GI endoscopy hubs. Its Digestive Disease Institute offers advanced procedures including chromoendoscopy, endoscopic ultrasound (EUS), capsule endoscopy, and AI-supported colonoscopy. The center handles high-risk surveillance cases such as Barrett’s esophagus, hereditary CRC syndromes, and complex IBD follow-ups. Scope reporting is digitally integrated with histopathology and oncology services, making it ideal for patients requiring multi-disciplinary care.
Mediclinic City Hospital in Dubai Healthcare City maintains a strong GI program focused on early cancer detection and minimally invasive endoscopic therapeutics. The hospital uses Olympus EVIS EXERA III systems and offers CO₂ insufflation, polypectomy, band ligation, and mucosal resection services. Mediclinic’s patient portals allow same-day access to endoscopy reports, making it a preferred choice for busy professionals and corporate wellness packages.
American Hospital Dubai, an early adopter of capsule endoscopy and narrow-band imaging, remains a high-volume center for routine and complex procedures. Their gastroenterology unit includes sub-specialists for liver, biliary, and small bowel disorders, offering dual-scope evaluations and sedation care pathways for high-risk patients.
Burjeel Medical City in Abu Dhabi has developed an integrated digestive care model that includes robotic surgery, hepatology, and therapeutic endoscopy. Their team is known for handling tertiary referrals and post-transplant GI complications, especially in coordination with their oncology and interventional radiology units.
NMC Royal and Aster Hospitals, though positioned as mid-tier providers, have rapidly expanded their endoscopy infrastructure, with increasing adoption of AI-assisted colonoscopy systems and direct-access screening programs supported by major UAE insurers. These centers are often preferred for insured patients requiring routine scopes or basic diagnostic evaluations with fast-track approvals.
For patients seeking trusted specialist referrals, verified clinical listings, and appointment booking options across all major cities, platforms like HealthFinder.ae serve as a centralized gateway. Whether you’re exploring digestive health screening or looking for a second opinion, you can discover GI-focused hospitals and multi-specialty experts through their advanced search filters.
If you’re researching broader surgical specialties, including musculoskeletal consultations, the top orthopedic surgeons in Dubai are also profiled on HealthFinder with detailed insights into procedures, credentials, and clinic affiliations.
How to prepare mentally and physically for the procedure?
Preparing for an endoscopy or colonoscopy is not limited to following dietary restrictions or taking laxatives—it also involves managing expectations, understanding procedural flow, and reducing emotional resistance that may affect compliance. In the UAE’s diverse patient population, where language barriers, cultural hesitancies, and fear of sedation are common, mental and physical preparedness are equally important predictors of procedural success and diagnostic yield.
Physically, the preparation protocols vary depending on the procedure. For endoscopy, patients must fast for 6–8 hours—no food, milk, or juices—ensuring the stomach is empty for optimal visualization and to reduce the risk of aspiration under sedation. For colonoscopy, the focus is on complete bowel cleansing, typically involving split-dose polyethylene glycol (PEG) solution starting the evening before and early on the procedure day. Following a clear liquid diet for 24 hours is crucial. Patients should also discuss any ongoing medications—especially anticoagulants, diabetic medications, or antihypertensives—with their provider to ensure safe sedation and minimal bleeding risk.
Mentally, preparation starts with understanding that these procedures are routine, low-risk, and designed for early detection—not judgment or punishment. Many patients associate endoscopy or colonoscopy with discomfort, embarrassment, or the fear of discovering cancer. These anxieties are natural but can lead to unnecessary cancellations or incomplete preparation. UAE hospitals often use bilingual nurse educators, digital instruction videos, and pre-procedure counseling to normalize the experience and empower patient participation.
It helps to ask:
- What exactly will happen before, during, and after the procedure?
- What are the most common findings for someone with my symptoms?
- What will the results tell me, and what actions might follow?
Answering these questions upfront reduces ambiguity and increases the patient’s psychological readiness. Bringing a companion for support—especially for sedation recovery—can also reduce emotional burden and improve procedural adherence.
Patients are also advised to visualize the procedure as preventive, not reactive. Scopes are tools of control, not consequence. They allow for detection of early, reversible lesions long before symptoms escalate. This mental reframe from “fear of what might be found” to “certainty of what is ruled out” transforms passive apprehension into informed participation.
Lastly, adequate sleep the night before, wearing loose clothing, arriving early, and avoiding stimulants like coffee or nicotine on the day of the procedure help the body remain calm, responsive, and ready for sedation.
In structured GI centers across the UAE—whether private hospitals in Dubai or government facilities in Abu Dhabi—patients who enter the procedure physically prepared and mentally aligned consistently report higher satisfaction, better scope tolerance, and faster post-procedure recovery. Preparation isn’t just a checklist—it’s a mindset.
Can diet, lifestyle, or stress influence GI symptoms that lead to these tests?
Yes. Diet, lifestyle, and psychological stress can all induce gastrointestinal symptoms that mimic those caused by organic diseases—and often serve as the initial trigger for a referral to endoscopy or colonoscopy. In UAE healthcare practice, where clinicians must differentiate functional GI disorders from structural or inflammatory pathologies, recognizing the influence of non-disease factors is critical. Scopes are not only used to detect pathology, but also to rule it out—especially in patients whose symptoms persist despite normal labs, imaging, or empirical treatment.
Dietary patterns in the UAE—high in processed foods, low in fiber, and rich in saturated fats—can lead to bloating, constipation, and dyspepsia. Spicy foods, caffeine, soft drinks, and fast-eating behaviors contribute to reflux symptoms, postprandial fullness, and gastric discomfort. These symptoms often mimic gastritis or peptic ulcer disease, prompting referrals for upper GI endoscopy. In younger patients, normal endoscopic findings commonly point to functional dyspepsia, where lifestyle adjustment—not medication—is the actual solution.
Sedentary lifestyle and erratic meal timing also contribute to sluggish bowel motility, gas retention, and altered stool patterns—often confused with early colonic disease or IBS (Irritable Bowel Syndrome). While colonoscopy may be used to rule out inflammatory bowel disease (IBD), colorectal polyps, or malignancy, the end result in many such cases is a diagnosis of functional bowel disorder, with no visible abnormality.
Psychological stress and anxiety, particularly in high-performance environments like Dubai and Abu Dhabi, activate the gut-brain axis, leading to real, measurable symptoms such as cramps, bloating, urgency, and nausea. This is not imagined illness—it is neurogastroenterology in action. Patients with stress-induced GI symptoms often undergo both upper and lower scopes to rule out red-flag pathology. When scopes return normal, clinicians pivot toward biofeedback, stress management, dietary therapy, or low-dose neuromodulators.
It’s important to note that lifestyle-induced GI symptoms and disease-caused symptoms can overlap. For instance, a patient with ulcerative colitis may be symptomatically triggered by dietary lactose, while a patient with normal colonoscopy may have severe pain from visceral hypersensitivity caused by stress. This overlap is what makes endoscopy and colonoscopy invaluable—they help clinicians separate functional mimicry from organic evidence, allowing for targeted therapy.
In the UAE’s expat-rich population, where dietary habits vary by ethnicity, and stress levels run high due to relocation, work-life imbalance, and medical mistrust, functional GI symptoms are frequent and often indistinguishable from disease without visual inspection.
Ultimately, scopes are not always ordered to confirm pathology—they are often performed to exclude it, allowing clinicians to shift the management plan toward lifestyle correction rather than pharmacologic escalation.
Choosing the Right Diagnostic Scope in UAE’s Gastrointestinal Landscape
Endoscopy and colonoscopy are more than diagnostic procedures—they are decision frameworks that help UAE clinicians translate patient symptoms into structured, visual evidence. While endoscopy focuses on the upper GI tract, colonoscopy targets the lower digestive system—each with its own preparation, scope, technology, and clinical context. Whether the goal is to investigate unexplained symptoms, screen for cancer, or manage chronic conditions like IBD, these procedures offer real-time diagnosis, tissue sampling, and in many cases, immediate therapeutic action.
In the UAE, the integration of advanced platforms such as AI-assisted lesion detection, CO₂ insufflation systems, and digital EMR reporting has made both scopes not only safer, but faster and more accurate. The country’s structured referral pathways, bilingual care teams, and insurance-aligned preventive screening protocols ensure that patients receive the right scope—at the right time—with the right follow-up.
Patients should not view endoscopy or colonoscopy as intimidating interventions, but rather as tools of diagnostic clarity and control. Proper mental preparation, adherence to dietary and medication guidelines, and open communication with care teams increase the likelihood of smooth recovery and actionable results.
For those seeking expert guidance, HealthFinder.ae offers a centralized platform to explore GI specialists, view hospital profiles, and book consultations across major UAE cities. Whether you’re searching for gastroenterologists or related specialties such as orthopedic surgeons in Dubai.
Endoscopy and colonoscopy are not just procedures—they are entry points into personalized digestive care, and in the UAE, they are delivered with global precision and regional cultural sensitivity.
Fathima Kausar K is a contributing writer at HealthFinder.ae, where she works on health-related articles that help readers understand medical topics in a simple, clear, and practical way. Her role focuses on researching and writing content that explains health conditions, medical procedures, diagnostic tests, and treatment options in language that everyday readers can understand.
She works closely with structured medical sources and published references, turning complex healthcare information into easy-to-read articles while maintaining accuracy and clarity. Her writing is focused on helping people make informed decisions by understanding symptoms, terminology, and care options before speaking with healthcare professionals.
Fathima’s approach is careful, reader-first, and clarity-driven. She focuses on accuracy, structure, and readability rather than technical jargon, so readers can confidently navigate health topics without confusion. Through her work at HealthFinder, she contributes to making medical information more accessible, understandable, and trustworthy for a wider audience.