In the UAE, non-alcoholic fatty liver disease (NAFLD) has become a silent epidemic—impacting a growing number of both Emirati and expat populations. Driven by modern lifestyle factors like obesity, insulin resistance, and sedentary habits, NAFLD now ranks among the most common liver conditions nationwide. Unlike alcohol-related liver disease, NAFLD develops in those who drink little or no alcohol but still face the risk of serious liver damage—from simple fat buildup (steatosis) to inflammation (NASH), fibrosis, and even cirrhosis.
As of 2025, healthcare authorities in the UAE—including DHA, SEHA, and private centers—have adopted more advanced, UAE-specific protocols for early detection. These involve a combination of BMI tracking, SGPT/ALT enzyme monitoring, glucose levels, and imaging techniques like FibroScan. Persistently high ALT levels—especially above 45 U/L in males or 34 U/L in females—are a critical red flag when paired with metabolic risk markers.
Whether you’re a concerned patient or a clinician shaping care pathways, this guide decodes the latest NAFLD strategies in the UAE. We’ll explore diagnostic protocols, local lab thresholds, diet plans, and how early lifestyle changes can transform outcomes.
Understanding NAFLD – Definition, Stages & UAE Relevance
Non-alcoholic fatty liver disease (NAFLD) is a common liver condition where fat builds up in the liver cells of individuals who drink little to no alcohol. In the UAE, NAFLD has become increasingly prevalent due to high rates of obesity, type 2 diabetes, and inactive lifestyles—affecting both Emiratis and expatriates.
Understanding the stages of NAFLD is essential for early diagnosis and prevention, especially because most people experience no symptoms until the disease has advanced.
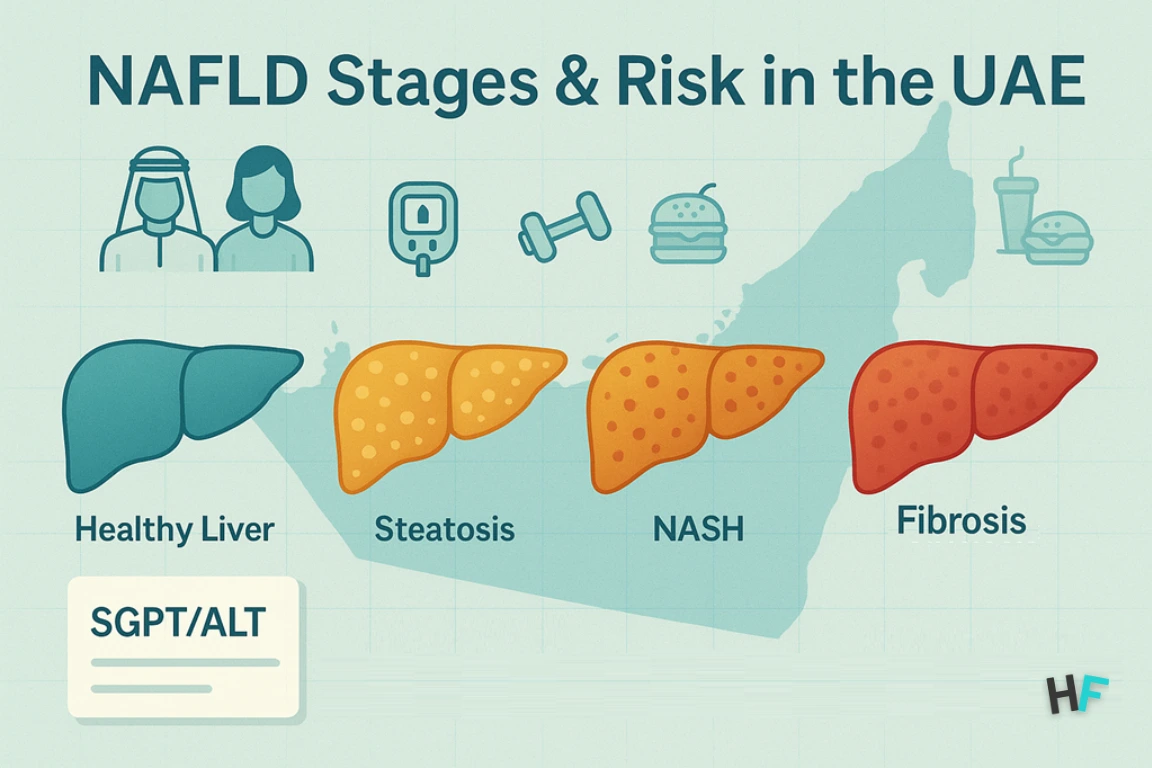
Stage 1: Simple Fatty Liver (Steatosis)
At this early stage, fat is present in liver cells but there’s no inflammation or damage. Most patients are unaware they have it, and it’s usually detected during routine blood tests. In UAE clinics, elevated liver enzymes—particularly SGPT (ALT)—often raise the first red flag.
Stage 2: Non-Alcoholic Steatohepatitis (NASH)
This stage involves liver inflammation and damage. Blood tests typically reveal higher SGPT levels, especially in patients with additional metabolic risks like high blood sugar or cholesterol. In the UAE, early-stage NASH is being identified more frequently due to proactive screening in high-risk individuals.
Stage 3: Fibrosis
Fibrosis means the liver has begun forming scar tissue due to ongoing damage. Although SGPT levels might normalize, internal damage progresses silently. This makes imaging tools like FibroScan, now commonly available at Aster, NMC, and SEHA facilities, crucial for accurate diagnosis.
Stage 4: Cirrhosis
At this advanced stage, the liver is severely scarred and its ability to function declines. Without proper treatment, patients face risks of liver failure or even liver cancer. Some cases may require a liver transplant, highlighting the importance of early intervention.
Early detection of NAFLD—especially using UAE-specific protocols like SGPT monitoring and FibroScan imaging—can prevent disease progression and avoid serious complications.
BMI & Waist Circumference: Key NAFLD Risk Factors in the UAE (2025)
When it comes to liver health in the UAE, stepping on the scale isn’t enough. Doctors now rely on two key metrics to detect non-alcoholic fatty liver disease (NAFLD) early: Body Mass Index (BMI) and waist circumference. These simple measurements can reveal hidden liver fat—even in people who feel healthy and have no symptoms.
BMI Cutoffs for NAFLD Screening in UAE Clinics
BMI is calculated using your height and weight, and helps estimate your body fat. In 2025, most UAE healthcare centers—including DHA and SEHA—use the following BMI scale for NAFLD risk:
| BMI (kg/m²) | Weight Category | NAFLD Risk Level |
|---|---|---|
| Under 23 | Healthy | Low risk |
| 23–24.9 | Overweight | Moderate risk |
| 25 or above | Obese | High risk |
For Arab and Asian populations, NAFLD can occur even at lower BMIs. That’s why UAE clinics start screening at 23, unlike the Western cutoff of 25.
Waist Circumference: A More Accurate Predictor of Liver Fat
Visceral fat (fat around your waist) is one of the strongest indicators of liver fat buildup. Even people with a normal BMI may have high liver fat if their waist size is above these thresholds:
| Waist Size | Gender | NAFLD Risk |
|---|---|---|
| ≥ 90 cm (35.4 in) | Men | Elevated |
| ≥ 80 cm (31.5 in) | Women | Elevated |
In the UAE, nutritionists, endocrinologists, and family doctors now measure waist circumference as part of annual checkups—especially for people with diabetes, PCOS, or sedentary office jobs.
NAFLD Can Happen Even If You’re Not Overweight?
This condition, called “lean NAFLD,” is becoming more common in the Gulf. That’s why doctors look at waist size + liver enzyme levels (like SGPT/ALT) to decide if liver imaging or a referral to a hepatologist is needed.
UAE clinics like Aster and LLH often combine:
- BMI
- Waist size
- Insulin resistance markers (like HOMA-IR) to detect NAFLD before symptoms even begin.
If you live in the UAE and your BMI is over 23 or your waist size is above the cutoff, don’t wait for liver symptoms. A simple SGPT blood test or ultrasound could catch liver fat early—when it’s still reversible through diet, exercise, and better blood sugar control.
| Activity | Goal | UAE Tip |
|---|---|---|
| Brisk Walking | 30–45 mins/day, 5x/week | Walk indoors (malls or gyms) in hot months |
| Resistance Training | 2–3x/week | Bodyweight or resistance bands at home |
| Break Sitting Time | 5–10 mins every hour | Set hourly reminders to stand/stretch |
| Total Movement | 150–180 mins/week | Reduces SGPT and improves blood sugar |
Bonus tip: Standing for 10 minutes after meals can reduce liver fat load.
2. Sleep: The Liver Repairs Itself While You Rest
Poor sleep increases cortisol, insulin resistance, and liver fat—even with a healthy diet.
| Sleep Habit | Target | Liver Impact |
|---|---|---|
| Sleep Duration | 7–9 hours/night | Supports liver cell repair and SGPT reduction |
| Sleep Timing | Sleep before 11 PM | Syncs with liver detox cycle and melatonin production |
| Screen Use | No screens 1 hour before bed | Balances fat-burning hormones (GH, leptin) |
| Sleep Apnea Screening | If overweight/snoring/tired AM | Untreated apnea worsens SGPT and fibrosis risk |
Many overweight UAE residents with high liver enzymes have undiagnosed sleep apnea—talk to your doctor if you feel tired despite 8 hours of sleep.
3. Supplements That Support Liver Health (UAE-Approved)
Supplements won’t reverse NAFLD on their own—but some may help reduce SGPT when used under a doctor’s supervision.
| Supplement | Typical Dose | Benefit |
|---|---|---|
| Vitamin E | 400–800 IU/day | Antioxidant; helps in non-diabetic NAFLD cases |
| Silymarin (Milk Thistle) | 140–420 mg/day | May reduce inflammation and liver enzymes |
| Omega-3 (EPA/DHA) | 1,000–2,000 mg/day | Lowers triglycerides and liver fat |
| Vitamin D3 | 2,000–5,000 IU/day | Often low in UAE; supports liver and metabolism |
| NAC (N-Acetylcysteine) | 600–1,200 mg/day | Boosts glutathione, a key liver antioxidant |
Always check with your UAE-based physician before starting supplements—especially if you’re on medications, pregnant, or diabetic.
NAFLD Recovery Formula = Movement + Sleep + Supplements
This formula highlights the three essential lifestyle pillars that work together to improve liver health and lower SGPT levels—without relying on medication.
| Lifestyle Pillar | Must-Do Habit | Liver Impact |
|---|---|---|
| Exercise | Walk 30+ mins/day, 5x/week | Lowers SGPT, burns liver fat |
| Sleep | Sleep 7–9 hrs/night, before 11 PM | Reduces insulin resistance, supports detox |
| Supplements | Use Vitamin E, D3, or Omega-3 if needed | May help normalize liver enzymes |
Glossary of NAFLD Terms in UAE Clinical Context (2025)
This glossary explains the key clinical terms, diagnostic tools, and institutional references used throughout the UAE’s NAFLD management protocols—helping patients and professionals stay aligned.
- NAFLD (Non-Alcoholic Fatty Liver Disease): A metabolic liver disorder where fat accumulates in liver cells in the absence of significant alcohol intake. Commonly linked with obesity, insulin resistance, and sedentary behavior—NAFLD is now among the most prevalent liver conditions in the UAE. Early detection using SGPT and FibroScan helps prevent its progression to more advanced stages.
- NASH (Non-Alcoholic Steatohepatitis): An inflammatory form of NAFLD where liver cells show signs of damage and scarring (fibrosis). NASH is considered a more severe stage and can lead to cirrhosis. In UAE protocols, NASH diagnosis is typically confirmed via elevated SGPT and liver stiffness assessment through FibroScan.
- SGPT (ALT – Alanine Aminotransferase): A liver-specific enzyme used in UAE hospitals to detect liver cell injury. SGPT levels >34 U/L in women or >45 U/L in men are clinical red flags. It’s one of the most sensitive early markers for fatty liver screening in wellness packages, diabetes checkups, and visa medicals.
- FibroScan: A non-invasive ultrasound-based imaging test that evaluates liver stiffness and fat content. UAE facilities like Aster, NMC, SEHA, and Burjeel use FibroScan to assess fibrosis stage and guide NAFLD management.
- HbA1c (Hemoglobin A1c): A blood marker showing average blood glucose over 2–3 months. Frequently included in NAFLD workups in the UAE to assess insulin resistance—a key driver of liver fat accumulation.
- MRI-PDFF (Proton Density Fat Fraction MRI): An advanced MRI-based scan offering precise quantification of liver fat. Used for patients with suspected NASH or fibrosis when ultrasound or FibroScan is inconclusive. Available at major UAE tertiary hospitals.
- DHA (Dubai Health Authority): The regulatory health body overseeing public and private clinical services in Dubai. DHA clinical guidelines influence NAFLD protocols in government clinics via the NABIDH health information exchange system.
- SEHA (Abu Dhabi Health Services Company): Abu Dhabi’s primary public health operator, managing hospitals and clinics. SEHA’s use of the Malaffi digital platform ensures NAFLD alerts and lab result tracking across Abu Dhabi healthcare providers.
- Visceral Obesity: Fat stored around abdominal organs (not just under the skin), strongly associated with metabolic syndrome and liver fat buildup. Common in normal-BMI individuals in the Gulf region—contributing to “lean NAFLD.”
FAQs – Common Questions About NAFLD, SGPT & Liver Healing in the UAE?
Here are the most frequently asked questions UAE patients ask their doctors about non-alcoholic fatty liver disease (NAFLD) and SGPT (ALT) levels—answered with practical, up-to-date insights based on UAE clinical protocols.
What is a dangerously high SGPT level?
ALT above 100 U/L is considered significantly elevated and may suggest:
- NASH (non-alcoholic steatohepatitis)
- Drug-induced liver injury
- Early fibrosis or scarring
In UAE clinics: >45 U/L in men or >34 U/L in women usually triggers follow-up tests like FibroScan or MRI-PDFF.
Can NAFLD be reversed without medication?
Yes. In early stages, NAFLD is 100% reversible through:
- Losing 7–10% of body weight
- Daily walking or movement
- Cutting refined carbs and sugary foods
Most UAE patients see SGPT normalize in 3–6 months of consistent lifestyle change.
How do I know if my fatty liver is getting worse?
Watch for:
- SGPT keeps rising despite effort
- FibroScan shows liver stiffness >F2 stage
- Ongoing fatigue or upper abdominal pressure
- High insulin resistance or blood sugar
Your doctor may refer you to a hepatologist if these signs appear.
Are supplements like milk thistle or vitamin E safe?
Yes, if supervised by a doctor.
- Vitamin E: Proven to reduce inflammation (used in non-diabetic cases)
- Milk Thistle (Silymarin): Natural antioxidant, mild liver support
- Omega-3: Lowers triglycerides and liver fat
Always check with a DHA or SEHA doctor before starting supplements, especially if on medication.
I have a normal BMI. Can I still have fatty liver?
Yes—this is called lean NAFLD.
Even with a BMI <23, liver fat can build up due to:
- High waist circumference
- Sedentary work
- Sugary diets and soft drinks
This is common in young adults in the UAE.
How often should I recheck my SGPT levels?
- Mild elevation (35–60 U/L) → Repeat in 3 months
- >100 U/L or worsening → Get liver imaging + referral immediately
Can intermittent fasting help reverse NAFLD?
Yes, when done correctly.
Popular protocols like 14:10 or 16:8 can:
- Lower insulin resistance
- Reduce liver fat
- Improve inflammation markers
Many UAE clinics now guide fasting under nutritionist supervision—especially for overweight men and women with PCOS.
Where can I get tested for fatty liver and SGPT in the UAE?
NAFLD diagnosis and FibroScan are available at:
- Aster Hospitals & Clinics (Dubai, Sharjah)
- LLH, Burjeel, Medeor (Abu Dhabi, Al Ain)
- NMC & Mediclinic (nationwide)
- DHA Clinics via NABIDH system
- SEHA facilities via Malaffi referral
Dr. Aisha Rahman is a board-certified internal medicine specialist with over 12 years of clinical experience in chronic disease management and preventive healthcare. She has worked at leading hospitals across the UAE, helping patients manage conditions such as diabetes, hypertension, cardiovascular diseases, and metabolic disorders.
A strong advocate for preventive medicine, Dr. Rahman emphasizes early diagnosis, lifestyle modifications, and patient education to reduce chronic illness risks. She is an active member of the Emirates Medical Association and has contributed to health awareness programs and medical research initiatives. Her expertise has been featured in The National UAE, Gulf Health Magazine, and leading medical journals. As a keynote speaker at healthcare conferences, she shares insights on evidence-based treatments, patient-centered care, and advancements in internal medicine.
Dr. Omar Al-Farsi is a clinical nutritionist and medical researcher with over 15 years of experience in dietary science, metabolic disorders, and preventive healthcare. He has served as a senior consultant for UAE healthcare authorities and contributed to public health initiatives focused on nutrition education and disease prevention.
Dr. Al-Farsi has collaborated with leading hospitals, research institutions, and universities in the UAE, ensuring that health information is scientifically accurate and evidence-based. His research has been published in Gulf Medical Journal, Dubai Health Review, and WHO Nutrition Reports, making significant contributions to nutrition science and public health awareness.