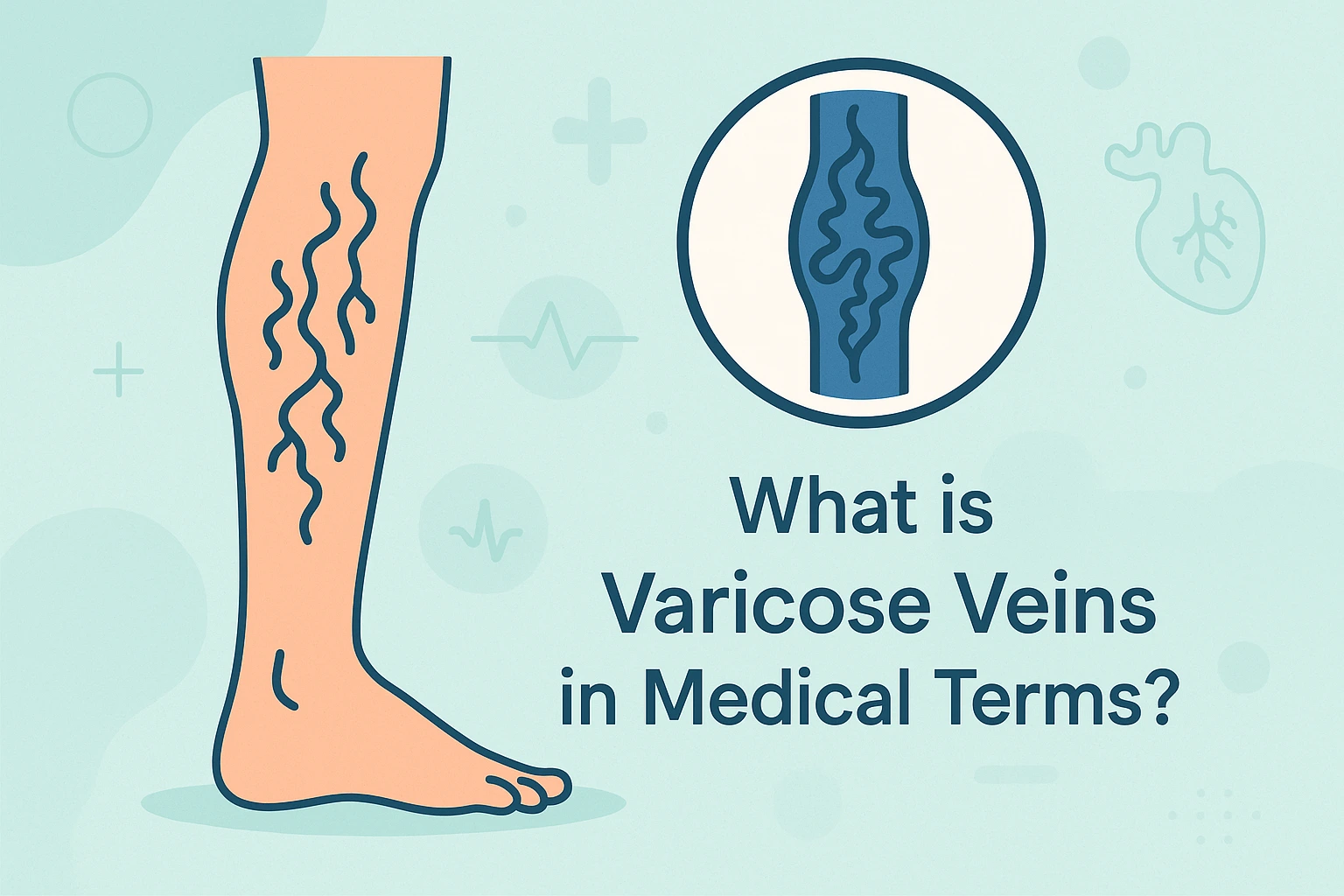
Varicose veins are swollen, twisted veins that are visible just beneath the surface of the skin. They commonly occur in the legs and feet, where the veins are under the most pressure. Normally, veins have one-way valves that prevent blood from flowing backward. When these valves weaken or become damaged, blood can pool in the veins, causing them to enlarge and become twisted. While varicose veins are usually not a serious health concern, they can cause discomfort and lead to complications such as pain, swelling, and skin ulcers.
Causes and Risk Factors of Varicose Veins
Varicose veins are often caused by increased pressure on the veins, leading to a breakdown in the vein’s valve system. The key factors contributing to the development of varicose veins include:
- Age: As people age, the veins lose elasticity and the valves may weaken, making it harder for blood to flow upward against gravity.
- Genetics: A family history of varicose veins increases the likelihood of developing them.
- Gender: Women are more likely to develop varicose veins due to hormonal changes, particularly during pregnancy, menopause, or while using birth control pills.
- Pregnancy: The increased blood volume and pressure on the veins during pregnancy can cause varicose veins, though they often improve after childbirth.
- Obesity: Excess weight puts added pressure on the veins in the lower body, increasing the risk of developing varicose veins.
- Prolonged standing or sitting: Occupations or lifestyles that involve long periods of standing or sitting without moving can cause blood to pool in the veins, contributing to varicose veins.
- Previous blood clots: History of blood clots or deep vein thrombosis (DVT) can damage the veins and contribute to varicose vein formation.
- Hormonal changes: Hormones relax the vein walls, increasing the risk of developing varicose veins, especially during pregnancy or menopause.
Symptoms of Varicose Veins
Varicose veins can cause a range of symptoms, from mild discomfort to more serious complications. Common symptoms include:
- Visible, bulging veins that are blue or purple in color, most often on the legs.
- Pain or a feeling of heaviness in the legs, especially after standing for long periods.
- Swelling in the feet and ankles.
- Itching, burning, or cramping in the affected area.
- Skin discoloration or ulcers near the varicose veins, particularly if left untreated for long periods.
- Tiredness or aching in the legs, which may worsen after standing or sitting for prolonged periods.
Diagnosis and Treatment of Varicose Veins
Varicose veins are diagnosed through a physical exam, where a healthcare provider will inspect the veins and ask about symptoms. Additional diagnostic tests, such as ultrasound, may be used to assess blood flow and determine the severity of the condition.
Treatment options depend on the severity of the varicose veins and the symptoms they cause. Common treatments include:
- Lifestyle changes: Simple changes like regular exercise, weight management, and elevating the legs can help alleviate symptoms and prevent progression.
- Compression stockings: These help improve blood flow and reduce swelling by applying gentle pressure to the legs.
- Sclerotherapy: A procedure in which a solution is injected into the varicose veins, causing them to collapse and fade over time.
- Laser therapy: A minimally invasive treatment that uses focused light to close off small varicose veins.
- Endovenous laser treatment (EVLT): A procedure where a laser is used to close off the vein, which is then reabsorbed by the body.
- Vein stripping or surgery: In more severe cases, surgery may be needed to remove or tie off the problematic veins.
Prevention and Management of Varicose Veins
While varicose veins cannot always be prevented, several strategies can reduce the risk or ease the symptoms:
- Stay active: Regular exercise, particularly activities like walking, helps improve circulation and prevent blood from pooling in the veins.
- Maintain a healthy weight: Reducing excess weight reduces the pressure on the veins in the lower body.
- Elevate the legs: Elevating your legs when resting helps improve blood flow and reduce swelling.
- Avoid prolonged periods of standing or sitting: Take breaks to move around and stretch, particularly if you have a job that requires you to stand or sit for extended periods.
- Wear compression stockings: These help prevent varicose veins from worsening and reduce swelling in the legs.
When to Seek Medical Help for Varicose Veins?
If you experience severe pain, swelling, or if you develop ulcers or skin changes near varicose veins, it’s important to consult a healthcare provider. Untreated varicose veins can lead to complications such as blood clots, skin ulcers, or bleeding. Early diagnosis and treatment can help manage symptoms and prevent further damage.
Related Terms to Varicose Veins
FAQs for Varicose Veins
When should I go to the ER for varicose veins?
If you experience severe pain, swelling, or any signs of complications like fainting or chest pain, seek emergency care.
How can heat and dehydration affect varicose veins?
In hot weather, dehydration can worsen symptoms of varicose veins, especially during long-haul flights or fasting periods.
What are some ways to reduce the risk of varicose veins?
Maintaining a healthy weight, staying active, and avoiding prolonged periods of standing can help reduce risk.
